Cardiovascular Disease in HIV
The increased risk of cardiovascular disease in people with HIV and specific strategies to treat it. This presentation discusses potential mechanisms, comorbidity gaps, and the impact of traditional risk factors. Explore the role of inflammation and immune dysfunction in atherosclerosis and vulnerable plaque formation.
- cardiovascular disease
- HIV
- increased risk
- treatment strategies
- comorbidity gaps
- traditional risk factors
- inflammation
- immune dysfunction
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
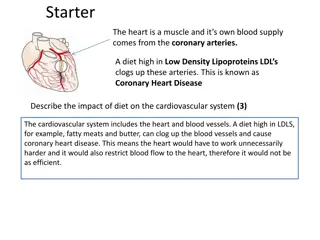
Cardiovascular Disease in HIV Steven K. Grinspoon, MD Professor of Medicine Harvard Medical School Boston, Massachusetts
Financial Relationships With Ineligible Companies (Formerly Described as Commercial Interests by the ACCME) Within the Last 2 Years: Dr Grinspoon has served as a consultant to Theratechnologies and ViiV Healthcare. (Updated 02/17/23) Slide 2
Learning Objectives After attending this presentation, learners will be able to: Describe the degree and potential mechanisms of increased risk of cardiovascular disease in PWH Describe specific strategies that may be of use to treat cardiovascular disease in PWH Slide 3
Life Expectancy and Comorbidity Gaps Persist Total years HIV- 9 yrs HIV+ Comorbidity*- free years HIV- 15 yrs HIV+ *Chronic liver, kidney, or lung disease; diabetes; cancer; cardiovascular disease Marcus JAMA Netw Open 2020 Slide 4
CVD Risk in PWH is Increased Beyond That Predicted by Traditional Risk Factors Global Meta-analysis PWH In the VACS cohort, the HR of MI was 1.48 in HIV vs. non-HIV adjusting for FRS, and comorbidities, (95% CI 1.27-1.72). Slide 5
Increased Traditional Risk Factors Account for Only a Portion of CVD Risk in HIV A 12 Hypertension RR 1.75 P<0.0001 10 Events Per 1000 PYs 8 Diabetes 6 4 Dyslipidemia 2 0 0 5 10 15 20 25 HIV Non-HIV HIV+ non-HIV+ DM, HTN, and dyslipidemia, though increased, accounted for 25% of excess risk Newer studies suggest importance of inflammation and immune dysfunction, as non traditional risk factors Triant JCEM 2007 Slide 6
Immune Activation Relates to Novel Atherosclerotic Phenotype in HIV Recent studies in HIV+ patients without known CVD, demonstrate that atherosclerotic plaques are: Non-calcified, high risk morphology features (vulnerable) Associated with inflammation and immune activation In the general population, inflamed, non-calcified, and high-risk morphology plaque is more prone to rupture. MI results from rupture of vulnerable plaque in 75% of cases Slide 7
Increased High Risk Morphology Plaque in HIV Patients Mean minimal attenuation < 40 Hounsefield Units LOW ATTENUATION PLAQUE (LAP) % of subjects with high risk morphology plaque RC A Plaque segment / reference segment > 1.05 POSITIVELY REMODELED (PR) PLAQUE RC A Naghavi Circ 2003, Schoenhanger Circ 2000 &JACC 2001; Zanni AIDS 2013 Slide 9
Increased Aortic 18FDG PET Uptake in HIV Control HIV 3.0 p = 0.0003 p = 0.0003 2.5 Aortic TBR 2.0 1.5 1.0 CVD Controls HIV FRS -Matched Controls Subramanian JAMA 2012 Slide 10
Activated Monocytes Are Present at Surface of High Risk Plaque and Accumulate FDG Tahara Nat Med 2014 Slide 11
Newer Modalities Suggesting Increased Coronary Inflammation: Reduced PCAT Density 12 Foldyna CROI 2023 Slide 12
A New Paradigm for Atherogenesis in HIV Persistent Viral Replication Microbial Translocation T-cell activation Monocyte Activation RCA High Risk Plaque Inflammation Slide 13
Current Challenges in Preventing and Treating CHD in HIV Identifying patients with disease: current risk identification strategies are not adequate Understanding the optimal timing and use of ART to maximize effects on immune function and minimize metabolic effects Developing a safe and effective strategy for primary prevention, especially for those not identified by current algorithms, but with substantial subclinical disease Developing an intervention that addresses both traditional and immune-related risk factors Slide 14
Immune Activation Improves with ART but Does not Normalize and Inflammation Persists 35 P = 0.008 %Activated CD8+ T Cells (HLA- 30 DR+ CD38+CD8+) 25 20 15 10 5 0 HIV+ at Baseline HIV+ after Treatment Healthy Control Zanni JAMA Cardiology 2016 Slide 15
Potential Interventions For CVD in HIV Traditional Risk Modification Strategies - Antihypertensive - Antidiabetic - Lipid Lowering - ASA Immune/Inflammatory Modulators - ART - Statins - Mineralocorticoid Receptor Antagonists - CCR5, IL Antagonists Slide 16
Traditional Risk Modification Strategies in HIV Lifestyle Improves waist circumference, BP, Glucose, no event data Lipid Lowering- Most successful strategies target LDL Statins reduce LDL and coronary plaque in HIV- event trial ongoing, NCT02344290 PCSK9 inhibitors lower LDL in non HIV, improve inflammation, no event data Blood pressure lowering Few studies, no event data Blood Glucose lowering Metformin improves glucose, coagulation, inflammatory markers, weight, no event data ASA Underutilized in HIV, even among those at high risk, no prospective event data Fitch AIDS 2006, Lo Lancet HIV 2015, Hadigan JAMA 2000, Triant OFID 2014 Slide 17
RAAS Blockade Improves Microvascular Perfusion and Vascular Inflammation Srinivasa CROI 2023 18 Slide 18
Need for a Large RCT to Inform Clinical Practice HIV patients with low traditional risk scores are at increased risk for CVD with subclinical plaque and inflammation ART alone is not enough to prevent CVD in PWH 19 Slide 19
Statins in HIV Generally safe and well tolerated in smaller studies; newer statins do not aggravate glucose Effectively lower LDL Decrease inflammatory pathways May hve effects on non CVD events Silverberg Ann Int Med 2009, Moncunill AIDS 2005, Negredo AIDS 2006 Slide 20
Statins Address Both Traditional and Immune Risk Factors in HIV LDL Lowering: Statins lower LDL by similar amounts in patients with and without HIV: (HIV- infected: -26.2%; HIV-uninfected: -26.9%) Dampening of Immune Activation: Decrease monocyte activation reflected in decreased circulating levels of sCD14 and the macrophage-derived phospholipase Lp-PLA2 Silverberg Ann Int Med 2009, McComsey CROI 2013, Funderburg JAIDS ePUB Slide 21
Newer Statins Do Not Increase Glucose Nor Interact with PI s Drug PI Effects on Glucose LDL Lowering and Dose Interaction Pravastatin (40 mg/d) - - -33 mg/dL, -25% Atorvastatin (20 to 40 mg/d) + +/- -38 mg/dL, -29% Rosuvastatin (10 mg/d) + + -28 mg/dL -28% Pitavastatin (4 mg/d)* - - -48 mg/dL, -28% Pitavastatin metabolized primarily by glucoronidation. Minimally metabolized by CYP3A. No known interactions with antiretroviral therapy no dose limitations. Included in 2013 ACC/AHA guidelines as a recommended moderate dose statin. *Among dyslipidemic patients with high starting cholesterol levels. Sponseller CROI 2014, Aberg Endo 2013, Eckard JID 2014, Stone JACC 2013 Slide 22
Statins Reduce Vascular Events in Non HIV Patients with Low LDL and Increased CRP Events/100p-y: Placebo: 1.36 Rosuva: 0.77 HR 0.56 LDL was reduced 47 mg/dL and should have resulted in a HR of 0.73 based on LDL lowering alone, according to CTTC meta-analysis. Instead, JUPITER showed a HR of 0.56, greater than expected based on LDL lowering alone Ridker N Engl J Med 2008; CTTC Lancet 2010 Slide 23
Many HIV Patients with High-Risk Plaque would not Receive Recommendation for Statin by Newest AHA Guidelines CHD risk underestimated by traditional risk scores Zanni AIDS 2014 Slide 25
Statin Effects on Coronary Artery Plaque in HIV p = .009 p < .0001 p = .005 110 40 20 p = .009 p < .0001 p = .005 90 20 0 Absolute Change in Direct LDL (mg/dL) Change in Lp-PLA2 Noncalcified Plaque Percent Change in 70 0 -20 50 (ng/mL) 30 -20 -40 10 -40 -60 -10 -30 -60 -80 -50 -80 -100 Placebo Atorvastatin Placebo Atorvastatin Placebo Atorvastatin Decreasing non-calcified plaque in proximal left anterior descending (LAD) coronary artery in patient on atorvastatin for 12 months. Lo Lancet HIV 2015 Slide 26
Dampening of Immune Activation May Reduce Risk of non-CHD Events in HIV Data from HIV studies: Modest improvement in creatinine clearance Possible decreased risk of cancers Reduced mortality among HIV in non-randomized studies (HR 0.33, P=0.009) Longenecker 2014, Overton CID 2013, Galli AIDS 2014, Moore PLOS One 2011 Slide 27
110+ Sites Across US, Canada, Spain, Thailand, Brazil, South Africa, Zimbabwe, Uganda, Botswana, Peru, India, and Haiti. Recruitment Closed in 2019 www.reprievetrial.org KowaGilead ViiV Slide 28
Where Are We in REPRIEVE? Recruited over 7700 participants from more than100 sites and 12 countries Events driven trial with accrual of 75% of events Mean duration of participation 5.75 yrs, Excellent retention, drop out < 5/100 PY Slide 29
REPRIEVE Clinical Sites Over 100 clinical sites globally Slide 30 30-KF
Study Schema Screening and Consent Asymptomatic people with HIV, at low to moderate traditional CVD risk R N=7769 Randomization Pitavastatin Placebo Intervention N=800, 2 yrs Mechanistic Study Mechanistic Primary Endpoint Coronary plaque, vascular Inflammation, immune activation Clinical Primary Endpoint CVD Death Unstable Angina Arterial Revasc PAD MI TIA & Stroke Slide 31
Study Population Inclusion Criteria Documented HIV infection Receiving stable ART CD4+ > 100 cells/mm3 Age 40 years, 75 years No ASCVD 10-yr ASCVD risk score <7.5% LDL < 190 mg/dL 7.5% and 10% LDL, < 160 mg/dL >10% and 15%, LDL < 130 mg/dL Exclusion Criteria Current use of statins, gemfibrozil, or PCSK9 inhibitors Known decompensated cirrhosis Slide 32
Baseline Characteristics Characteristic Total (7770) 5,352 (69%) 2,418 (31%) 4.5 (2.1-7.0) Natal sex Male, N (%) Female, N (%) ASCVD risk score (%), total population LDL (mg/dL) Age (years) Race 108 (87,128) 50 (45-55) 2,705 (35%) 3,366 (43%) 1,139 (15%) 560 (7%) White, N (%) Black/AA, N (%) Asian, N (%) Other, N (%) Slide 33
How Has REPRIEVE Informed Our Knowledge of CVD in HIV? Slide 34
The Mechanistic Substudy Will Determine Key Factors Contributing To CVD In PWH 755 participants Mean age: 51 years, 23% natal female, median ASCVD risk score: 5.0% 48% had coronary plaque, including 30% with very low ASCVD risk (<5%) 23% had vulnerable plaque features present IL-6, oxLDL, IL-6 and LpPLA2 associated with plaque JAMA Open 2021 Hoffmann Am Heart J 2019; JAMA Network Open 2021 Slide 35
Preliminary Comparison of REPRIEVE with Data from SCAPIS and PROMISE Karady et al. ACC 2023 Slide 36
Baseline Whole Exome Sequencing Performed in REPRIEVE Assess how polygenic risk scores and Clonal Hematopoiesis of Indeterminate Potential (CHIP) relate to MACE and statin effects on MACE in PWH Bhatacharya CROI 2023 Slide 37
Conclusions and Future Directions Modulation of traditional and nontraditional risks is necessary to prevent CVD in HIV; ART with viral suppression is likely not enough New therapies tested in large RCT s are necessary prevent and treat excess CVD in PWH REPRIEVE will assess a statin strategy for primary CVD prevention in HIV and inform us of risk factors which predict MACE and plaque progression Slide 38
Thank You to Our Site PIs, Study Teams, Trial Networks, Funders and Participants NEAT Trial Network ACTG Canadian HIV Trial Network Non ACTG REPRIEVE Sites Kowa ViiV Healthcare Gilead Slide 39