Acute inflammation
Acute inflammation is a protective response of the body to injury, intertwined with the repair process. It can be categorized into acute and chronic types based on the duration. The causes of inflammation vary from bacterial and viral infections to chemical exposure and radiation. The cardinal signs of acute inflammation include redness (rubor), heat (calor), swelling (tumor), and loss of function (unctio laesa). Understanding the basis of these signs involves increased blood flow, vascular permeability, chemical mediators, and nerve stimulation. Components of acute and chronic inflammation involve various cellular responses, particularly polymorphonuclear leukocytes. These visual aids provide insights into the complexity of the inflammatory process.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acute inflammation Assist. Prof.Dr. Baydaa H. Abdullah
Inflammation Is a protective response The body s response to injury Interwoven with the repair process
Inflammation Types Acute (sec, mins, hrs) Chronic (days, weeks, months, yrs)
Causes of inflammation Bacterial Viral Protozoal Metazoal Fungal Immunological Tumours Chemicals, toxins etc Radiation
Inflammation The Cardinal Signs of Acute Inflammation RUBOR CALOR TUMOR FUNCTIO LAESA
Inflammation The basis of the five cardinal signs Increased blood flow due to vascular dilatation gives redness and heat. Increased vascular permeability gives oedema causing tissue swelling. Certain chemical mediators stimulate sensory nerve endings giving pain. Nerves also stimulated by stretching from oedema. Pain and swelling result in loss of function. 2nd Yr Pathology 2010
Components of acute and chronic inflammation 2nd Yr Pathology 2010
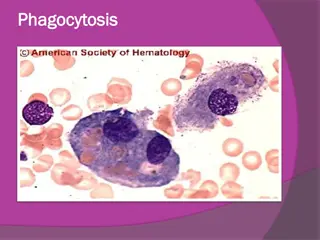
Cell of the acute inflammatory response Polymorphonuclear leukocyte
The phases of inflammation FIRST THERE IS VASCULAR DILATATION followed by exudation of protein-rich oedema fluid which floods the area, dilutes toxins, allows immunoglobulins to opsonise bacteria and provides substrate (fibrinogen) for fibrin scaffold. SECOND THERE IS ACTIVE EMIGRATION OF POLYMORPHS through vessel wall and along the chemotactic gradient to the site of injury
The phases of inflammation Fluid escapes from vessels because of endothelial cell (EC) retraction, opening up gap-junctions. The vessels which are normally involved are the post-capillary venules where the EC have high affinity receptors for histamine. THE VASCULAR PHASE OF INFLAMMATION Severe EC injury leads to leakiness of all vessels capillaries, venules and arterioles - giving acute local oedema, e.g. blister formation after a burn.
PHAGOCYTOSIS Recognition and attachment Foreign objects coated with opsonins IgG and C3b which attach to receptors on polymorph surface. Engulfment Cell membrane fuses around an object: at the some time lysosomes empty into the vacuole, often before vacuole has time to seal - this gives rise to 'regurgitation during feeding' and enzymatic damage to surrounding tissue. Killing or degradation H2O2, hypohalous acid (HOC1) produced by myeloperoxidase and superoxides kill bacteria. Lysozyme digests them. 2nd Yr Pathology 2010
Summary of acute inflammation Stimulated by physical injury, infection, foreign body Resident macrophages and/or damaged endothelium, mast cells IL-1, TNF, endothelin, histamine Vascular response: vasodilation, endothelial contraction, exudation of plasma Neutrophils: marginate (selectin-glycoprotein), adhere (integrin-CAM), extravasate (CD31), migrate (IL-8, chemotactic stimuli) Phagocytosis: recognition, engulfment, killing Phagocytosis receptors bind mannose, oxidized lipids, lipopolysaccharides, lipoteichoic acids, opsonins Killing is O2-dependent (respiratory burst, NADPH oxidase generated H2O2; myeloperoxidase generated HOCl; iNOS generated NO) or independent (lysozyme, lactoferrin, defensins) Responding leukocytes cause pain and loss-of-function via prostaglandins, enzymes Complete resolution; fibrosis, organization or scarring; abcess formation; progression to chronic inflammation
Outcomes of Acute Inflammation Resolution of tissue structure and function with elimination of stimulus Tissue destruction and persistent inflammation Abscess pus-filled cavity (neutrophils, monocytes and liquefied cellular debris) walled off by fibrous tissue and inaccessible to circulation tissue destruction caused by lysosomal and other degradative enzymes Ulcer loss of epithelial surface acute inflammation in epithelial surfaces Fistula abnormal communication between organs or an organ and a surface Scar Causes distortion of structure and sometimes altered function Chronic inflammation Marked by replacement of neutrophils and monocytes with lymphocytes, plasma cells and macrophages Accompanied by proliferation of fibroblasts and new vessels with scarring
Outcomes of Acute Inflammation Resolution of tissue structure and function with elimination of stimulus Tissue destruction and persistent inflammation Abscess pus-filled cavity (neutrophils, monocytes and liquefied cellular debris) walled off by fibrous tissue and inaccessible to circulation tissue destruction caused by lysosomal and other degradative enzymes Ulcer loss of epithelial surface acute inflammation in epithelial surfaces Fistula abnormal communication between organs or an organ and a surface Scar Causes distortion of structure and sometimes altered function Chronic inflammation Marked by replacement of neutrophils and monocytes with lymphocytes, plasma cells and macrophages Accompanied by proliferation of fibroblasts and new vessels with scarring
Outcomes Resolution The complete restoration of the inflamed tissue back to a normal status. Inflammatory measures such as vasodilation, chemical production, and leukocyte infiltration cease, and damaged parenchymal cells regenerate. In situations where limited or short lived inflammation has occurred this is usually the outcome. Fibrosis Large amounts of tissue destruction, or damage in tissues unable to regenerate, can not be regenerated completely by the body. Fibrous scarring occurs in these areas of damage, forming a scar composed primarily of collagen. The scar will not contain any specialized structures, such as parenchymal cells, hence functional impairment may occur.
Outcomes Abscess formation A cavity is formed containing pus, an opaque liquid containing dead white blood cells and bacteria with general debris from destroyed cells. Chronic inflammation In acute inflammation, if the injurious agent persists then chronic inflammation will ensue. This process, marked by inflammation lasting many days, months or even years, may lead to the formation of a chronic wound. Chronic inflammation is characterised by the dominating presence of macrophages in the injured tissue. These cells are powerful defensive agents of the body, but the toxins they release (including reactive oxygen species) are injurious to the organism's own tissues as well as invading agents. Consequently, chronic inflammation is almost always accompanied by tissue destruction.
Patterns of Inflammation Serous Inflammation Marked by outpouring of thin fluid From blood serum, e.g. burn blisters Effusion from mesothelial cells lining the pleural, peritoneal and pericardial cavity Fibrinous Inflammation A feature of pericardial and peritoneal inflammation Vascular permeability allows larger molecules like fibrin to pass or procoagulant stimulus exists in the interstitium (e.g. cancer cells) Suppurative Inflammation Characterized by production of large amount of pus composed of neutrophils, necrotic cells and edema fluid Involves pyogenic bacteria e.g. Streptococci and Staphylococcus aureus Abscesses are focal localized collections of purulent inflammatory tissue caused by suppuration. Ulcers Local defect or excavation of the surface of an organ or tissue by sloughing of inflammatory necrotic tissue Acute stage - intense polymorphonuclear infiltration and vascular dilation in margin Chronic stage - margin and base develop fibroblastic proliferation, scarring and accumulation of lymphocytes, plasma cells and macrophages
Systemic inflammatory response Acute Phase Response Fever Acute-phase protein secretion from liver Leukocytosis Tachycardia, increased blood pressure Shivering, chills Anorexia, somnolence, malaise Septic shock