Candidiasis: Symptoms, Causes, and Treatment
Candidiasis is an infection caused by the yeast Candida albicans and can manifest in various forms in the oral cavity. Learn about the different types of candidiasis, common symptoms, risk factors, and treatment options for this fungal infection.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
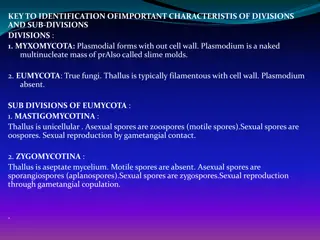
CANDIDIASIS Infection with the yeastlike fungal organism Candida albicans is termed candidiasis C. albicans may exist in two forms(dimorphism) The yeast form ---> relatively innocuous, The hyphal form --->usually associated with invasion of host tissue.
Candidiasis : most common oral fungal infection in humans C. albicans : normal oral microflora(30% to 50% of people without clinical evidence of infection.) three general factors: I. The immune status of the host 2. The oral mucosal environment 3. The strain of C. albicans
Pseudomembranous candidiasis (thrush) Erythematous candidiasis
The best recognized form of candidal infection adherent white plaques that resemble cottage cheese or curdled milk on the oral mucosa Can be removed by scraping them with a tongue blade or dry gauze sponge The underlying mucosa may appear normal or erythematous. bleeding --->probably another process, such as lichen planus or chemotherapy.
broad-spectrum antibiotics (acute) 1. 2. by impairment of the patient's immune system. (leukemic patients, HIV) (chronic) Symptoms(if present ):mild,burning sensation , unpleasant taste (salty or bitter). Site: buccal mucosa, palate, and dorsal tongue
do not show white flecks or a white component is not a prominent feature.
1-acute atrophic candidiasis (antibiotic sore mouth) Patients complain: burning sensation like if a hot beverage had scalded it diffuse loss of the filiform papillae of the dorsal tongue, resulting in a reddened, "bald tongue
2- central papillary atrophy of the tongue ( median rhomboid glossitis) asymptomatic and chronic was thought to be a developmental defect of the tongue a well demarcated erythematous zone that affects the midline, posterior dorsal tongue The erythema is due in part to the loss of the filiform papillae. The lesion is usually symmetric with smooth to lobulated surface Often the mucosal alteration resolves with antifungal therapy
Some patients with central papillary atrophy +other Sites chronic multifocal candidiasis. Sites: junction of the hard and soft palate and the angles of the mouth. "kissing lesion
The involvement of the angles of the mouth(angular cheilitis, perleche) is characterized by erythema, fissuring, and scaling older person with VD severity of the lesions waxes and wanes. 20% albicans, 60% C. albicans & Staphylococcus aureus, , 20% are S. aureus cheilocandidiasis
Denture stomatitis erythematous candidiasis, chronic atrophic candidiasis varying degrees of erythema, sometimes accompanied by petechial hemorrhage in denture- bearing areas of a maxillary removable prosthesis Although C. albicans is often associated with this condition,biopsy specimens of denture stomatitis seldom show candidal hyphae actually penetrating the keratin layer of the host epithelium.
a white patch that cannot be removed by scraping The least common anterior buccal mucosa cannot clinically be distinguished from a routine leukoplakia Often the leukoplakia with candidal infection red and white areas(speckled leukoplakia ) increased frequency of epithelial dysplasia
Severe oral candidiasis as a component of a relatively rare group of immunologic disorders The immune problem usually becomes evident during the first few years of life:candidal infections of the mouth, nails, skin, and other mucosal surfaces. The oral lesions : thick, white plaques that typically do not rub off (essentially chronic hyperplastic candidiasis).
Patients should be evaluated periodically because any one of endocrine abnormalities (endocrinecandidiasis syndrome), as well as iron-deficiency anemia, may develop in addition to the candidiasis. endocrine disturbances: hypothyroidism, hypoparathyroidism, hypoadrenocorticism (Addison's disease), and diabetes mellitus. Prevalence of oral cancers
periodic acid-Schiff (PAS) method the candidal hyphae and yeasts The PAS method stains carbohydrates of fungal cell walls( the bright magenta color ) diagnosis of candidiasis: hyphae or pseudohyphae
parakeratin elongation of the epithelial rete ridges a chronic inflammatory cell infiltrate in the connective tissue immediately subjacent to the infected epithelium neutrophils microabscesses often in the parakeratin layer and the superficial spinous cell layer near the organisms The candidal hyphae are embedded in the parakeratin layer and rarely penetrate into the viable cell layers of the epithelium unless the patient is extremely immunocompromised.
Nystatin: suspension or pastille bitter taste, disguised with sucrose If the candidiasis is due to xerostomia ---> Absorbtion in the GI tract: poor ---> effectiveness depends on direct contact---> multiple daily doses
Amphotericin B : intravenous treatment of life-threatening systemic fungal infections. Clotrimazole: not well absorbed ---> several times each day. pleasant- tasting troche (lozenge) Clotrimazole cream : effective treatment for angularcheilitis because this drug has antibacterial and antifungal properties.
Ketoconazole: the first antifungal drug that could be absorbed across the GI Tract single daily dose & oral route of administrationhave been noted an acidic environment is required for proper absorption liver toxicity FDA: ketoconazole should not be used as initial therapy for routine oral candidiasis Fluconazole more effective than ketoconazole well absorbed systemically, and an acidic environment is not required for absorption once-daily dosing liver toxicity is rare resistance to the drug seems to develop in some instances.