Diabetic Ketoacidosis during Pregnancy
Diabetic ketoacidosis (DKA) during pregnancy is a serious condition with potential risks for both mother and fetus. This metabolic emergency is characterized by hyperglycemia and metabolic acidosis due to elevated ketone bodies. Learn about the incidence, pathogenesis, clinical features, diagnosis, investigations, and management of DKA in pregnant women to ensure optimal care and outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Diabetic Ketoacidosis during Pregnancy By Dr: Anisa Al-harazi
Diabetic Ketoacidosis: A metabolic emergency in which hyperglycemia is associated with a metabolic acidosis due to greatly raised ketone bodies. Is a life-threatening condition for the mother and the fetus. Incidence: 2 - 9 % of diabetic pregnant women. Maternal mortality 4 15 %. Fetal mortality 30 90 %.
DKA : is More commonly seen in type I DM . More common during pregnancy due to raised insulin resistance and lipolysis that lead to uncontrolled hyperglycemia especially if associated with conditions of excessive stress like : - Diarrhea or hyperemesis. - infection or any febrile illness. -use of corticosteroid or B2 agonist. -prolonged fasting or starvation.
Pathogenesis : Gluconeogenesis and glycogenolysis Stress ketones Glucose glycosuria Metabolic acidosis Osmotic diuresis vomiting D Dehydration ehydration
Dehydration Dehydration Renal hypo perfusion Impaired excretion of ketones and H.inos Hyperventilation (Kussmaul s breathing) Maternal and fetal Distress.
Clinical features: Start with extreme thirst and frequent urination. Prostration , nausea , vomiting and abdominal pain. Dry skin and mouth . Body temperature is subnormal even in infection. Tachycardia , hypotension. Hyperventilation (air hunger Kussmaul respiration ). Smell of aceton on breath. In severe condition the ventilation decreases due to respiratory depression. Confusion , stuper or even coma.
diagnosis Is made when: Blood glucose >250 mg /dl. Ketone bodies in blood and urine. Arterial PH < 7.3 Serum bicarbonate < 15 meq /L.
Investigations: Blood glucose level. CBC. Blood gases . Urea and electrolytes. Urine analysis. Blood and urine culture. Chest X.R. ECG.
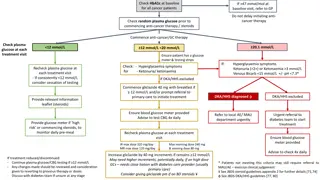
Management: The principles of management: Replace fluid losses. Replace deficient insulin. Careful attention to electrolytes. Restore the acid-base balance. Replace the energy losses. Seek the underlying cause. Continuous fetal monitoring.
Management: No time should be lost and treatment is started as soon as the first blood sample has been taken. Fluid replacement : Fluid deficit as much as 6 - 7 L must replaced in 12 24 h. One liter of N.S.in one hour then 500ml/h till pulse and BP back to normal. Add KCI 20mmol to each liter.
Management: Insulin: Start 0.2u/Kg iv. bolus then 0.1u/Kg/h in N.S. If blood glucose not fall 30% in 3 hours then drip rate is doubled. When B.G near 200mg/dl, N.S is changed to 5% dextrose. Continuous infusion 12 - 24 hours after resolution of ketosis.
Management: Place in left lateral position. Broad spectrum antibiotics. Nasogastric tube if coma. CVP line in shocked patient. Heparin. Measure the fluids to avoid pulmonary or cerebral edema. Supplement oxygen. Monitor urine output.
Monitor blood glucose hourly. If PH <7.0 give bicarbonate. Continuous fetal monitoring. Enquiry into the cause and treat it.