Diabetic Ketoacidosis
Diabetic Ketoacidosis (DKA) is a serious complication of diabetes characterized by high blood sugar, acidic ketones, and dehydration. This condition is triggered by factors like insulin deficiency, illness, infections, and stress. The role of insulin is crucial in managing glucose levels and preventing the accumulation of ketone bodies. Counterregulatory hormones play a role in DKA by increasing insulin resistance and activating processes like glycogenolysis and gluconeogenesis. Recognizing the signs and symptoms of DKA, such as fruity breath, dehydration, and altered mental status, is essential for timely diagnosis and treatment. Laboratory findings in DKA include hyperglycemia, anion gap acidosis, and ketone presence in urine and serum.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
DKA Precipitating Factors Failure to take insulin Failure to increase insulin Illness/Infection Pneumonia MI Stroke Acute stress Trauma Emotional Medical Stress Counterregulatory hormones Oppose insulin Stimulate glucagon release Hypovolmemia Increases glucagon and catecholamines Decreased renal blood flow Decreases glucagon degradation by the kidney
Diabetic Ketoacidosis Due to: Severe insulin deficiency Excess counterregulatory hormones Glucagon Epinephrine Cortisol Growth hormone
Role of Insulin Required for transport of glucose into Muscle Adipose Liver Inhibits lipolysis Absence of insulin Glucose accumulates in the blood Liver Uses amino acids for gluconeogenesis Converts fatty acids into ketone bodies Acetone, Acetoacetate, -hydroxybutyrate Increased counterregulatory hormones
Counterregulatory Hormones - DKA Increases insulin resistance Activates glycogenolysis and gluconeogenesis X X X Activates lipolysis Inhibits insulin secretion Epinephrine X X X Glucagon Cortisol X X Growth Hormone X X
Insulin Deficiency Glucose uptake Lipolysis Proteolysis Free Fatty Acids Glycerol Amino Acids Gluconeogenesis Glycogenolysis Hyperglycemia Ketogenesis Acidosis Osmotic diuresis Dehydration
Signs and Symptoms of DKA Polyuria, polydipsia Enuresis Dehydration Tachycardia Orthostasis Abdominal pain Nausea Vomiting Fruity breath Acetone Kussmaul breathing Mental status changes Combative Drunk Coma
Lab Findings Hyperglycemia Anion gap acidosis (Na + K) (Cl + Bicarb) >12 Bicarbonate <15 mEq/L pH <7.3 Urine ketones and serum ketones Hyperosmolarity
Differential Diagnosis Anion Gap Acidosis Alcoholic ketoacidosis Lactic acidosis Renal failure Ethylene glycol or methyl alcohol poisoning Starvation in late pregnancy or lactation (rare)
Atypical Presentations DKA can be present with BS <300 Impaired gluconeogenesis Liver disease Acute alcohol ingestion Prolonged fasting Insulin-independent glucose is high (pregnancy) Chronic poor control but taking insulin Bedside urine ketones false negatives Measure acetoacetate not -hydroxybutyrate Send blood to lab
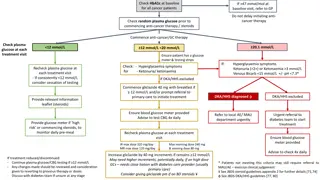
Treatment of DKA Fluids and Electrolytes Fluid replacement Restores perfusion of the tissues Lowers counterregulatory hormones Average fluid deficit 3-5 liters Initial resuscitation 1-2 liters of normal saline over the first 2 hours Slower rates of 500cc/hr x 4 hrs or 250 cc/hr x 4 hours When fluid overload is a concern If hypernatremia develops NS can be used
Treatment of DKA Fluids and Electrolytes Hyperkalemia initially present Resolves quickly with insulin drip Once urine output is present and K<5.0, add 20-40 meq KCL per liter. Phosphate deficit May want to use Kphos Bicarbonate not given unless pH <7 or bicarbonate <5 mmol/L
Treatment of DKA Insulin Therapy IV bolus of 0.1-0.2 units/kg (~ 10 units) regular insulin Follow with hourly regular insulin infusion Glucose levels Decrease 75-100 mg/dl hour Minimize rapid fluid shifts Continue IV insulin until urine is free of ketones
Treatment of DKA Glucose Administration Supplemental glucose Hypoglycemia occurs Insulin has restored glucose uptake Suppressed glucagon Prevents rapid decline in plasma osmolality Rapid decrease in insulin could lead to cerebral edema Glucose decreases before ketone levels decrease Start glucose when plasma glucose <300 mg/dl
Insulin-Glucose Infusion for DKA Blood glucose <70 70-100 101-150 151-200 201-250 251-300 301-350 351-400 401-450 451-500 >500 Insulin Infusion 0.5 units/hr 1.0 2.0 3.0 4.0 6.0 8.0 10.0 12.0 15.0 20.0 D5W Infusion 150 cc/hr 125 100 100 75 50 0 0 0 0 0
Complications of DKA Infection Precipitates DKA Fever Leukocytosis can be secondary to acidosis Shock If not improving with fluids r/o MI Vascular thrombosis Severe dehydration Cerebral vessels Occurs hours to days after DKA Pulmonary Edema Result of aggressive fluid resuscitation Cerebral Edema First 24 hours Mental status changes Tx: Mannitol May require intubation with hyperventilation
Once DKA Resolved Treatment Most patients require 0.5-0.6 units/kg/day Pubertal or highly insulin resistant patients 0.8-1.0 units/kg/day Long acting insulin 1/2-2/3 daily requirement NPH, Lente, Ultralente or Lantus Short acting insulin 1/3-1/2 given at meals Regular, Humalog, Novolog Give insulin at least 2 hours prior to weaning insulin infusion.
Prevention of DKA Sick Day Rules Never omit insulin Cut long acting in half Prevent dehydration and hyperglycemia Monitor blood sugars frequently Monitor for ketosis Provide supplemental fast acting insulin Treat underlying triggers Maintain contact with medical team
Hyperosmolar Non-ketotic Syndrome Extreme hyperglycemia and dehydration Unable to excrete glucose as quickly as it enters the extracellular space Maximum hepatic glucose output results in a plateau of plasma glucose no higher than 300-500 mg/dl When sum of glucose excretion plus metabolism is less than the rate which glucose enters extracellular space.
Hyperosmolar Non-ketotic Syndrome Extreme hyperglycemia and hyperosmolarity High mortality (12-46%) At risk Older patients with intercurrent illness Impaired ability to ingest fluids Urine volume falls Decreased glucose excretion Elevated glucose causes CNS dysfunction and fluid intake impaired No ketones Some insulin may be present Extreme hyperglycemia inhibits lipolysis
Hyperosmolar Nonketotic Syndrome Presentation Extreme dehydration Supine or orthostatic hypotension Confusion coma Neurological findings Seizures Transient hemiparesis Hyperreflexia Generalized areflexia
Hyperosmolar Nonketotic Syndrome Presentation Glucose >600 mg/dl Sodium Normal, elevated or low Potassium Normal or elevated Bicarbonate >15 mEq/L Osmolality >320 mOsm/L Creatinine may increased
Hyperosmolar Nonketotic Syndrome Treatment Fluid repletion NS 2-3 liters rapidly Total deficit = 10 liters Replete in first 6 hours Insulin Make sure perfusion is adequate Insulin drip 0.1U/kg/hr Treat underlying precipitating illness
Clinical Errors Fluid shift and shock Giving insulin without sufficient fluids Using hypertonic glucose solutions Hyperkalemia Premature potassium administration before insulin has begun to act Hypokalemia Failure to administer potassium once levels falling Recurrent ketoacidosis Premature discontinuation of insulin and fluids when ketones still present Hypoglycemia Insufficient glucose administration
Conclusion Successful management requires Judicious use of fluids Establish good perfusion Insulin drip Steady decline Complete resolution of ketosis Electrolyte replacement Frequent neurological evaluations High suspicion for complications Determine etiology to avoid recurrent episodes