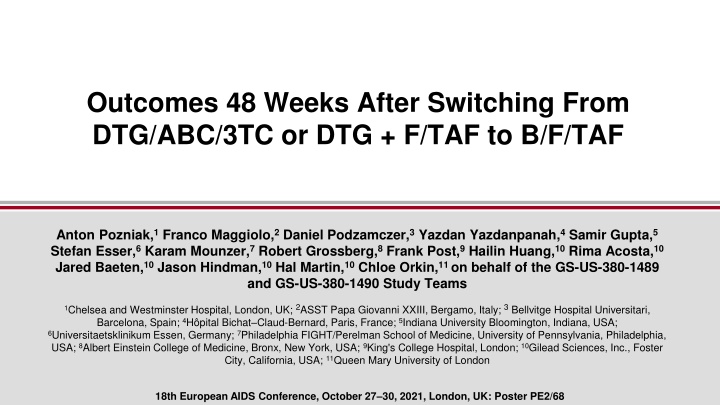
Outcomes 48 Weeks After Switching From DTG/ABC/3TC or DTG + F/TAF to B/F/TAF
This study examines the outcomes of HIV patients switching from DTG/ABC/3TC or DTG+F/TAF to B/F/TAF after 48 weeks. Results are presented by a diverse group of medical professionals from various institutions across different countries. The findings shed light on the effectiveness and safety of the treatment transition in managing HIV.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Outcomes 48 Weeks After Switching From DTG/ABC/3TC or DTG + F/TAF to B/F/TAF Anton Pozniak,1Franco Maggiolo,2Daniel Podzamczer,3Yazdan Yazdanpanah,4Samir Gupta,5 Stefan Esser,6Karam Mounzer,7Robert Grossberg,8Frank Post,9Hailin Huang,10Rima Acosta,10 Jared Baeten,10Jason Hindman,10Hal Martin,10Chloe Orkin,11 on behalf of the GS-US-380-1489 and GS-US-380-1490 Study Teams 1Chelsea and Westminster Hospital, London, UK; 2ASST Papa Giovanni XXIII, Bergamo, Italy; 3Bellvitge Hospital Universitari, Barcelona, Spain; 4H pital Bichat Claud-Bernard, Paris, France;5Indiana University Bloomington, Indiana, USA; 6Universitaetsklinikum Essen, Germany; 7Philadelphia FIGHT/Perelman School of Medicine, University of Pennsylvania, Philadelphia, USA; 8Albert Einstein College of Medicine, Bronx, New York, USA; 9King's College Hospital, London;10Gilead Sciences, Inc., Foster City, California, USA; 11Queen Mary University of London 18th European AIDS Conference, October 27 30, 2021, London, UK: Poster PE2/68
Introduction Bictegravir (B; BIC)/emtricitabine (F; FTC)/tenofovir alafenamide (TAF; B/F/TAF) is a guidelines-recommended, single-tablet regimen for people with HIV-1 (PWH)1-3 B/F/TAF has a high barrier to resistance, favorable drug-drug interaction profile, and ability to be given once daily without food restrictions Safety and efficacy through Week 144 have been demonstrated in two Phase 3 studies (GS-US-380-1489 [ClinicalTrials.gov NCT02607930] and GS-US-380-1490 [NCT02607956]) of B/F/TAF compared with 3-drug dolutegravir (DTG) containing regimens in treatment-na ve adults4-8 All participants were offered enrollment in an open-label extension (OLE) after completing 144 wk of the randomized portions of the studies 2
Objective To evaluate 48-wk outcomes on B/F/TAF in an OLE that followed 144 wk of blinded DTG- based treatment in two Phase 3 studies of treatment-na ve PWH 3
Study Designs: Randomized, Double Blind, Active Controlled 2 Endpoint 1 Endpoint 2 Endpoint 2 Endpoint Week 0 48 96 144 192 240 Treatment-Na ve Adults B/F/TAF qd n=314 Study 1489 HLA B*5701 negative Negative for chronic HBV eGFRCG 50 mL/min DTG/ABC/3TC placebo qd 1:1 Open-label B/F/TAF DTG/ABC/3TC qd n=315 B/F/TAF placebo qd Key inclusion criteria for both: No known resistance to FTC, TAF, ABC, or 3TC HIV-1 RNA 500 copies/mL B/F/TAF qd n=320 DTG + F/TAF placebo qd Study 1490 Chronic HBV or HCV infection allowed eGFRCG 30 mL/min 1:1 Open-label B/F/TAF DTG + F/TAF qd n=325 B/F/TAFplacebo qd 3TC, lamivudine; ABC, abacavir; eGFRCG, estimated glomerular filtration rate by Cockcroft-Gault equation; HBV, hepatitis B virus; HCV, hepatitis C virus; HLA, human leukocyte antigen. 4
Results: Participant Disposition From Baseline to Week 192 Study 1489 randomized: N=631 Study 1490 randomized: N=657 B/F/TAF: n=316* DTG/ABC/3TC: n=315 Treated B/F/TAF: n=320 DTG + F/TAF: n=325 D/C prior to Week 144, n (%) 55 (17) D/C prior to Week 144, n (%) 60 (19) 55 (17) 51 (16) n=259 n=260 Completed Week 144 n=260 n=274 Continued B/F/TAF n=252 Delayed switch to B/F/TAF n=254 Continued B/F/TAF n=254 Delayed switch to B/F/TAF n=265 Entered OLE n=254 Treated n=265 n=14 (6%) 6 5 1 1 1 D/C prior to Week 192 Participant decision Lost to follow-up Death Protocol violation Investigator s discretion n=11 (4%) 6 5 n=240 Completed Week 192 n=254 *2 participants randomized and not treated; 7 randomized and not treated; 5 randomized and not treated. D/C, discontinuation. 5
Characteristics at B/F/TAF Start* Study 1489 Study 1490 DTG/ABC/3TC B/F/TAF n=254 36 (22 71) DTG + F/TAF B/F/TAF n=265 38 (21 80) Median age, y (range) Female at birth, n (%) 29 (11) 26 (10) Race/ethnicity, n (%) Black or African descent 94 (37) 80 (30) Hispanic/Latinx ethnicity 54 (21) 73 (28) Median body weight, kg (IQR) 83 (73, 94) 82 (71, 96) HIV-1 RNA 50 copies/mL, n (%) 9 (4) 2 (1) Median CD4 cells/ L (IQR) Asymptomatic HIV infection, n (%) 766 (599, 1023) 229 (90) 730 (550, 958) 234 (88) Median eGFRCG, mL/min (IQR) 116 (99, 138) 111 (95, 135) *All participants completed 144 wk on blinded DTG/ABC/3TC or DTG + F/TAF before entering OLE. CD4, cluster of differentiation-4; IQR, interquartile range. 6
Virologic Outcomes: Weeks 144192 HIV-1 RNA <50 Copies/mL Study 1489 Study 1490 100 100 100 99.6 99.6 99.2 99.2 99.2 98.0 96.5 100 100 99.2 98.9 98.4 96.5 96.6 94.9 93.3 92.8 80 80 84.5 83.5 Participants, % 60 60 40 40 DTG + F/TAF B/F/TAF DTG/ABC/3TC B/F/TAF 20 20 M=E M=F M=E M=F B/F/TAF Start B/F/TAF Start 0 0 Study Week 144 0 156 168 180 192 144 0 156 168 180 192 OLE Week 12 24 36 48 12 24 36 48 n=* 254 250 241 238 212 265 264 258 251 225 Participants who switched from DTG/ABC/3TC or DTG + F/TAF to B/F/TAF in the OLE maintained high levels of virologic suppression through Week 192/OLE Week 48 (M=E) Median CD4 changes from B/F/TAF start to Week 192/OLE Week 48, cells/ L (IQR): DTG/ABC/3TC B/F/TAF, -6 (-113, 104); DTG + F/TAF B/F/TAF, 14 (-83, 117) *Participants with nonmissing HIV-1 RNA at each visit. M=E, missing=excluded; M=F, missing=failure. 7
Virologic Resistance Through Week 192 Baseline Week 144 Week 144 Unblinding OLE B/F/TAF DTG/ABC/3TC DTG + F/TAF DTG/ABC/3TC DTG + F/TAF DTG/ABC/3TC B/F/TAF n=254 DTG + F/TAF B/F/TAF n=265 Participants, n n=315 n=325 n=269 n=281 Met criteria for resistance testing* 6 7 4 1 1 1 NRTI resistance detected 0 0 2 (M184V) 0 0 0 INSTI resistance detected 0 0 0 0 0 0 *Resistance testing performed for participants with confirmed HIV-1 RNA 200 copies/mL or 200 copies/mL at last visit, with no resuppression of HIV-1 RNA to <50 copies/mL while on study drug; 1 DTG/ABC/3TC participant developed M184V and had no resistance to integrase (IN); adherence by pill count was 93%; 1 DTG/ABC/3TC participant developed M184V and had assay failure for IN; adherence by pill count was 86%. INSTI, IN strand transfer inhibitor; NRTI, nucleoside reverse- transcriptase (RT) inhibitor. No resistance to any components of B/F/TAF occurred in any group Post-Week 144 but prior to switch, 2 participants on blinded study drug of DTG/ABC/3TC developed M184V, switched to B/F/TAF, and achieved HIV-1 RNA <50 copies/mL at their next visit 8
Adverse Events: Weeks 144192 DTG/ABC/3TC B/F/TAF n=254 73 3 Diarrhea (n=2), headache, abnormal dreams, alopecia, libido decreased, nausea, obesity, rash pruritic, and vomiting DTG + F/TAF B/F/TAF n=265 71 2 Diabetes mellitus, fatigue, flatulence, headache, lethargy, migraine, and weight decreased Participants, % Any AE Any study drug-related AE All occurred in 1 participant unless otherwise specified AE, adverse event. 9
Nausea Incidence and Prevalence Through Week 192* Prevalence Study drug-related prevalence Study 1489 Incidence Study drug-related incidence Study 1490 DTG/ABC/3TC B/F/TAF DTG + F/TAF B/F/TAF 20 20 15 15 Participants, % 10 10 5 5 3.7 0.7 0 0 0 0 Study Week 148 4 144 148 4 4 4 4 168 24 192 48 164 168 24 188 192 48 24 48 72 96 120 144 24 24 44 48 68 72 92 96 116 120 140 144 8 12 16 20 28 32 36 40 48 52 56 60 64 72 76 80 84 88 96 100 104 108 112 120 124 128 OLE Week 132 136 144 148 152 140 148 152 156 160 168 172 176 180 184 192 196 OLE Week n= 315 310 300 295 292 281 269 254 248 241 325 316 307 300 291 284 282 265 262 255 Among participants randomized to DTG/ABC/3TC (Study 1489) or DTG + F/TAF (Study 1490), the incidence and prevalence of nausea declined numerically after switching to B/F/TAF in the OLE *Hashmarks indicate transition from randomized phase to OLE; prevalence reset at OLE start. 10
Diarrhea Incidence and Prevalence Through Week 192* Prevalence Study drug-related prevalence Study 1489 Incidence Study drug-related incidence Study 1490 DTG/ABC/3TC B/F/TAF DTG + F/TAF B/F/TAF 20 20 15 15 Participants, % 10 10 5 5 1.1 0.4 0 0 0 0 Study Week 144 148 4 144 148 4 4 4 4 4 164 168 24 188 192 48 164 168 24 188 192 48 24 24 44 48 68 72 92 96 116 120 140 144 24 24 44 48 68 72 92 96 116 120 140 144 8 12 16 20 28 32 36 40 48 52 56 60 64 72 76 80 84 88 96 100 104 108 112 120 124 128 OLE Week 132 136 144 148 152 8 12 16 20 28 32 36 40 48 52 56 60 64 72 76 80 84 88 96 100 104 108 112 120 124 128 OLE Week 132 136 144 148 152 140 148 152 156 160 168 172 176 180 184 192 196 140 148 152 156 160 168 172 176 180 184 192 196 n= 315 310 300 295 292 281 269 254 248 241 325 316 307 300 291 284 282 265 262 255 Among participants treated with DTG/ABC/3TC or DTG + F/TAF, the incidence and prevalence of diarrhea declined numerically after switching to B/F/TAF in the OLE *Hashmarks indicate transition from randomized phase to OLE; prevalence reset at OLE start. 11
Adverse Events Leading to Discontinuation: Weeks 144192 1 participant who switched from DTG/ABC/3TC to B/F/TAF (Study 1489) died due to seizure unrelated to study drug on OLE Day 335/Study Week 192 12
Laboratory Abnormalities: Weeks 144192 DTG + F/TAF B/F/TAF n=265 14 DTG/ABC/3TC B/F/TAF n=254 8 Participants, % Any Grade 3 or 4 laboratory abnormality 2% in either group Nonfasting hyperglycemia 1 3 Increased fasting LDL 1 3 Glycosuria 1 2 LDL, low-density lipoprotein. 13
eGFR Changes: Weeks 144192 DTG/ABC/3TC B/F/TAF DTG + F/TAF B/F/TAF Study 1489 Study 1490 15 15 10 10 Median eGFRCG Change, 5 5 mL/min (IQR) +1 0 0 -0.4 -5 -5 -10 -10 B/F/TAF Start B/F/TAF Start -15 -15 Study Week 144 0 156 168 180 192 144 0 156 168 180 192 OLE Week 12 24 36 48 12 24 36 48 n=254 250 244 238 213 265 264 259 252 223 No reported cases of proximal renal tubulopathy or D/C due to renal AEs were observed on B/F/TAF 14
Weight Changes From Randomized Phase Baseline Through Week 192 Study 1489 Study 1490 7 6.1 5.9 6 1.1 5.0 OLE Median Weight Change 5 4.6 From Baseline, kg/y* 2.4 Week 1.0 0.3 1.1 192/OLE 48 144 4 0.9 0.4 OLE 1.2 0.7 0.4 3 1.1 96 48 2 0.8 3.0 2.9 2.7 1 1.6 0 B/F/TAF B/F/TAF DTG/ABC/3TC B/F/TAF DTG + F/TAF B/F/TAF Numerically greater weight changes were observed in those who switched from DTG/ABC/3TC (Study 1489) at OLE Week 48 postswitch than in those who switched from DTG + F/TAF (Study 1490): 2.4 vs 1.1 kg Switch from ABC to TAF has been associated with statistically significant weight gain, with one potential explanation being worse gastrointestinal tolerability with ABC vs TAF9,10 The difference in weight gain in Study 1489 at Week 48 (1.3 kg less with DTG/ABC/3TC) was similar to the difference in additional weight gain at OLE Week 48 (+1.4 kg when switching from DTG/ABC/3TC to B/F/TAF) 15 *Randomized phase baseline for all treatment groups.
Fasting Lipid Changes: Weeks 144192 DTG/ABC/3TC B/F/TAF LDL DTG + F/TAF B/F/TAF TG TC HDL TC:HDL 5 6 3.6 4.7 3.5 4.4 4 Median, mmol/L (IQR) 3.1 3.0 4 Median (IQR) 3 4.5 4.3 3.6 3.3 2 1.1 2.9 1.1 2.9 2 1.2 1.2 1 1.2 1.1 1.1 1.1 0 0 0 24 48 0 24 48 0 24 48 0 24 48 0 24 48 OL Week OL Week DTG/ABC/3TC B/F/TAF n=254 7 DTG + F/TAF B/F/TAF n=265 10 Participants, % Taking lipid-lowering agents at B/F/TAF start Initiated lipid-lowering agents while on B/F/TAF 2 4 Small changes in lipids were observed among participants who switched to B/F/TAF for 48 wk and small numbers of participants initiated lipid-lowering agents HDL, high-density lipoprotein; TC, total cholesterol; TG, triglycerides. 16
Conclusions Over 4 y of follow-up of treatment-na ve PWH who were initially randomized to DTG/ABC/3TC or DTG + F/TAF for 144 wk and then switched to 48 wk of OL B/F/TAF, we observed: High rates of virologic suppression with no treatment-emergent resistance to B/F/TAF Few AEs leading to D/C and no renal related D/Cs Declines in nausea and diarrhea incidence and prevalence after switching from DTG/ABC/3TC or DTG + F/TAF to B/F/TAF Small median lipid changes and minimal impact on TC:HDL ratio Numerically greater weight changes in those who switched from DTG/ABC/3TC than from DTG + F/TAF These results confirm the safety and efficacy of B/F/TAF among people who switch from DTG/ABC/3TC or DTG + F/TAF 17
References 1. DHHS. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents With HIV; 12/18/19; 2. EACS Guidelines Version 10.0 November 2019; 3. Saag MS, et al. JAMA 2018;320:379-96; 4. Gallant J, et al. Lancet 2017;390:2063-72; 5. Orkin C, et al. Lancet HIV 2020;7:e389-400; 6. Sax PE, et al. Lancet 2017;390:2073-82; 7. Stellbrink H-J, et al. Lancet HIV 2019;6:e364-72; 8. Wohl DA, et al. Lancet HIV 2019;6:e355-63; 9. Lakey W, et al. AIDS Res Hum Retroviruses 2013;29:435-40; 10. Sax PE, et al. Clin Infect Dis 2020;71:1379-89. 18
Acknowledgments We extend our thanks to the participants, their partners and families, and all GS-US-380- 1489 and GS-US-380-1490 investigators. Special thanks to the 1489 and 1490 study teams. These studies were funded by Gilead Sciences, Inc. 19
Backups 20
Fasting Lipid Changes: Weeks 144192 DTG/ABC/3TC B/F/TAF LDL DTG + F/TAF B/F/TAF TG TC HDL TC:HDL 250 5 3.6 3.5 181 171 200 4 Median, mg/dL (IQR) 99 101 117 Median (IQR) 119 150 3 175 3.6 165 3.3 100 2 114 112 48 48 101 96 50 1 47 46 0 0 0 24 48 0 24 48 0 24 48 0 24 48 0 24 48 OLE Week OLE Week DTG/ABC/3TC B/F/TAF n=254 7 DTG + F/TAF B/F/TAF n=265 10 Participants, % Taking lipid-lowering agents at B/F/TAF start Initiated lipid-lowering agents while on B/F/TAF 2 4 Small changes in lipids were observed among participants who switched to B/F/TAF for 48 wk and small numbers of participants initiated lipid-lowering agents HDL, high-density lipoprotein; TC, total cholesterol; TG, triglycerides. 21
Participants With Resistance US Black/African-American Woman Aged 46 Years GBR White Man Aged 24 Years DTG/ABC/3TC B/F/TAF DTG/ABC/3TC B/F/TAF 10000 1000000 VL: 5,650 copies/mL RT: none IN: S119P VL: 122,000 copies/mL RT: none IN: none 100000 HIV-1 RNA, Copies/mL VL: 2,660 copies/mL RT: M184V IN: none VL: 262 copies/mL RT: assay failure IN: assay failure VL: 279 copies/mL RT: M184V IN: assay failure 1000 10000 1000 100 50 100 50 10 10 0 24 48 72 96 120 144 168 192 216 240 0 24 48 72 96 120 144 168 192 216 240 Visit Week Visit Week VL, viral load. 22