Trimester Screening and Down Syndrome History
Explore the historical background of first-trimester screening and Down syndrome, from Langdon Down's theory to modern diagnostic techniques like amniocentesis and karyotyping. Learn about the genetics and maternal factors associated with this genetic condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
First trimester screening E.Keshavarz MD
Langdon Down (London 1866) Subgroup of idiots . Down syndrome(mongolian people) Down s theory:retrogression of ethnic type (Darwin s contemporary scientific reasoning for evolution) Theory was not true but 100 years later: Skin:dirty yellowish tinge skin and is deficient in elasticity,giving the appearance of being too large for the body
1866:congenital,dating from intrauterine life 1909:association with maternal age 1914:no increased within families 1914:syphilis,TB,epilepsy,alcholism,insanity,nervouse instability , endocrine abnormalities(thyroid , adrenal , pitiutary , thymus) 1932:diz.t:un.equally monoz.t:equally transmission from mother to the baby *** 1934:unequal migration of chromosomes during cell division trisomy
1960:familial Down syndrome translocation(15:21),no trisomy 1961:mosaism type of Down syndrome mosaism of normal and trisomic cells 1966:karyotyping of cultured amniotic fluid cells
Whole or a segment of long arm of ch 21 is in three copies: 1-non dysjunction(95%) 2-translocation 3-mosaicism 1991:95% of non dysjunction: maternal origin
Only amniocentesis ! 1-private health care system:>35 y was 5% now 10% and more! 2- NHS:5% pregnant mothers >37-40 y only 30% of trisomy 21 babies !
1970s 1970s 1980s 1980s 1990s 1990s 2000s 2000s
CRL measurement CRL measurements can be carried out transabdominally or transvaginally. A midline sagittal section of the whole embryo or fetus should be obtained.
NT measurement - CRL:45-84 mm (11w-13w 6d) -TAS(95% success)=TVS(other 5%) -Waiting for spontaneous fetal movement, asking the mother to cough, tapping the maternal abdomen(amnion membrane!)
NT measurement - Good work after 80-100 sonography and at least 10 min - Study on 100,000 cases:normal:1.2 (11w) to 1.9(13w 6d) abnormal:above the 95thcentile(>=3mm)
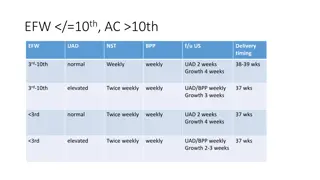
11-14 week sonography Trisomy 13 and Turner: mild growth restriction tachycardia(delay maturation of para.s ) Trisomy 18 and triploidy: mod-severe growth restriction bradycardia (early onset of growth restriction) Trisomy 21: normal growth mild increased in FHR (HF and compensatory increased FHR)
Type Type of aneuploidy of aneuploidy Free Free -hCG hCG PAPP PAPP- -A A Trisomy 21 Trisomy 21 Trisomy 18 & 13 Trisomy 18 & 13 Sex chromosomal anomalies Sex chromosomal anomalies Nl Nl Diandric triploidy Diandric triploidy Digynic triploidy Digynic triploidy
Down screening Triple test at 11w 13w 6d detection rate:90% Maternal serum biochemistry 16w detection rate:60% Combination of them:90%+(60% of other 10%) detection rate :96%
PAPP-A :lower in smoking and IVF Higher in black(60%) Free BHCG is more in 21 (than 18 and 13) specially in W13 PAPP-A is more in 21 (than 18 and 13) specially inW11 The difference is more in PAPP-A than Free BHCG Maternal serum biochemistry screening in W11 is better than W13 and also better in W10 than W11 W12 NT+W12 MSB:detection rate 84% W12 NT+W10 MSB:detection rate 94%
OSCAR OSCAR New methods of biochemical testing within 30 min(time- resolved-amplified-cryptate-emission)+ NT at the same time: One Step Clinics for Assessment of Risk
Maternal Maternal age+NT+FHR+FreeBHCG+PAPP age+NT+FHR+FreeBHCG+PAPP- -A A High 1.5% P 85% 21 >=1/50 CVS(70-90 day) Intermediate 15% p 14% 21 Detailed US for looking the new US markers <1/50,>1/1000 Low 83.5% p 1% 21 <=1/1000 US at W20
New US markers 1-NB 1-NB 2-Facial angle 2-DV PI 3-Ductus venusus flow 4-Trichospid flow 3-TR
Detection Detection Rate (%) (%) 30 30 Rate False Positive False Positive Rate (%) Rate (%) 5 5 Method of screening Method of screening MA MA MA + fetal NT MA + fetal NT 75 75- -80 80 5 5 MA + serum free MA + serum free -hCG & PAPP hCG & PAPP- -A A 60 60- -70 70 5 5 MA + NT + free MA + NT + free - -hCG & PAPP hCG & PAPP- -A (combined test) A (combined test) 85 85- -95 95 5 5 93 93- -96 96 2.5 2.5 Combined test + NB or TV flow or DV flow
Detection Detection Rate (%) Rate (%) False False Positive Positive Rate (%) Rate (%) 5 5 Method of screening Method of screening Combined test Combined test 90 90 Combined test + NB Combined test + NB 92 92 3 3 Combined test + FMF Angle Combined test + FMF Angle 92 92 3 3 Combined test Combined test + DV Flow + DV Flow 96 96 3 3 96 96 3 3 Combined test + TV Flow 94 94 2 2 Combined test + 2 additional markers 95 95 2 2 Combined test + 3 additional markers 96 96 2 2 Combined test + 4 additional markers
NB NB If NB is absent in 11 to 12 week: Patients are rescanned after 12 week and action is only taken at that point if there is persistence of the absence of the nasal bone.
Increased NT/ Abnormal reverse a wave in ductus In addition, there is an increased risk for cardiac defects and therefore such patients should have a follow up specialist fetal cardiac scan.
Combined and new markers in all fetuses One stage Time consuming Two stage(contingent policy) OSCAR Combined and new markers in intermediate group Cvs in high and anomaly scan in low CfDNA in intermediate........C vs in high and anomaly scan in low Combined+PLGF+ AFP+PAPPA.....ALS O DV PIV Modern contingent policy
Classic Markers Classic Markers Newer Markers Newer Markers Minor Minor Markers Markers (Less important) (Less important) Maxillary length Maxillary length Nasal Bone (NB) Nasal Bone (NB) Ductus Ductus Venosus Venosus Pulsatility Index Index for for Veins Veins (DV Pulsatility (DV PIV) PIV) Ear length Ear length Fronto Fronto- -Maxillary Angle Maxillary Angle (FMF angle) (FMF angle) Femur & humerus length Femur & humerus length Hepatic Hepatic Index Index (HA Artery Artery PI) Pulsatility Pulsatility (HA PI) Single umbilical artery Single umbilical artery Ductus Venosus (DV) Flow Ductus Venosus (DV) Flow Megacystis Megacystis Tricuspid Valve (TV) Flow Tricuspid Valve (TV) Flow Exomphalos Exomphalos Choroid plexus cysts Choroid plexus cysts Pyelectasis Pyelectasis Cardiac echogenic foci Cardiac echogenic foci
Preeclampsia Preeclampsia Preeclampsia, which affects about 2% of pregnancies, is a major cause of perinatal and maternal morbidity and mortality The likelihood of developing preeclampsia is increased by a number of factors in the maternal history, including Afro- Caribbean race, nulliparity, high body mass index and personal or family history of preeclampsia. However, screening by maternal history may detect only about 30% of those that will develop preeclampsia for a false positive rate of 5%.
measurement of the uterine artery pulsatility index (PI) at 11-13 weeks' gestation in combination with maternal history(inc) mean arterial pressure(inc) serum PAPP-A(dec >inc) placental growth factor (PLGF) (dec >inc) The factors in the maternal history that appear to make a significant independent contribution to the preeclampsia risk assessment included maternal BMI, age, ethnicity, smoking, and parity.
early rather than late preeclampsia is associated with an increased risk of perinatal mortality and morbidity and both short-term and long-term maternal complications. Combination of the above mentioned risk factors was shown to predict 90% of early preeclampsia, 35% of late preeclampsia, and 20% of gestational hypertension. This compares favorably with screening based on maternal history alone where only 30% of early and 20% of late preeclampsia are predicted for a 5% false positive rate.
Deciding whether to carry out prenatal invasive testing in pregnancies at risk of sex-linked genetic abnormalities Just necessary in male fetuses Angle between the genital tubercle & a horizontal line through the lumbosacral skin surface: Male if Female if > 30 Parallel or Convergent (< 20 )
Male Male assignment) Female Female Gestational Gestational Age Age (Wrong (Wrong assignment) (Wrong assignment) (Wrong assignment) 11 wks 11 wks 56% 56% 5% 5% 12 12 wks wks 3% 3% 0% 0% 13 13 wks wks 0% 0% 0% 0% o Test accuracy: 11 wks. 70.3% 12 wks. 98.7% 13 wks. 100% o In the male fetuses, there is a significant increase in the angle of the genital tubercle from the horizontal with CRL increment o Final decision should be undertaken only after 12 weeks