Doppler Studies in Pregnancy for Fetal Assessment
Explore the significance of Doppler studies in fetal assessment during pregnancy, including predictions of preeclampsia and fetal growth restriction, physiological changes in pregnancy, and the role of Doppler indices in umbilical artery assessment. Learn about uterine artery Doppler studies and physiological changes in pregnancy affecting arterial function.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
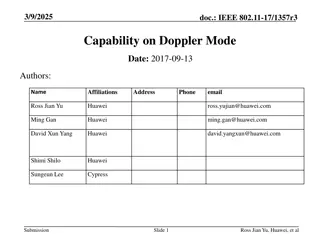
Doppler study in fetal assessment Doppler study in fetal assessment
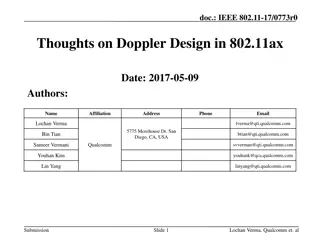
Doppler study in pregnancy Doppler study in pregnancy Uterine artery Prediction of preeclampsia Prediction of FGR diagnosis of FGR Umbilical artery (UA pulsatility index [PI] 95th) Fetal assessment in high risk pregnancies ( FGR , PE, AF abnormalities, ) Middle cerebral artery ( MCA PI 5thpercentile ) Fetal assessment in high risk pregnancies ( FGR , PE, AF abnormalities, ) Fetal anemia screening Ductus venosus FGR F/U
Physiological changes in pregnancy Physiological changes in pregnancy Basal arteries showed no changes, but spiral arteries were invaded by cytotrophoblastic cells and were converted into uteroplacental arteries. These have a dilated and tortuous lumen, a complete absence of muscular and elastic tissue, no continuous endothelial lining, mural thrombi and fibrinoid deposition. conversion of the spiral arteries to uteroplacental arteries is termed physiological change . : in two stages: the first wave of trophoblastic invasion converts the decidual segments of the spiral arteries in the first trimester the second wave converts the myometrial segments in the second trimester . As a result of this physiological change , the diameter of the spiral arteries increases from 15 20 to 300 500 mm, reducing impedance to flow
Uterine artery Doppler study Uterine artery Doppler study NORMAL IN 1TH : 2.35 NORMAL IN 1TH : 2.35 NORMAL IN 2TH : 1.44 NORMAL IN 2TH : 1.44
Umbilical artery Doppler Umbilical artery Doppler
Umbilical artery Doppler Umbilical artery Doppler Doppler indices UA Doppler waveform analysis is based upon the following characteristics of the maximum velocity envelope Peak systolic flow velocity (S) End-diastolic flow velocity (D) Average flow velocity over the cardiac cycle (A) These three values are used to develop indices that measure the pulsatility of the Doppler waveform reflecting the dynamic changes in flow through the cardiac cycle. The common Doppler indices used for obstetric applications are: Peak systolic to end-diastolic flow ratio (S/D) Pulsatility index (PI = S-D/A) Resistance index (RI = S-D/S) Doppler surveillance primarily benefited pregnancies complicated by fetal growth restriction (FGR) and/or hypertensive complications of pregnancy
MCA MCA
Middle cerebral artery Middle cerebral artery FETAL ANEMIA SCREENING : MCA-PSV is performed, when clinically indicated, after 20 weeks and before 34 weeks of gestation in the first affected pregnancy- results should be adjusted for gestational age. The optimal interval between examinations one to two week intervals based on clinical experience An MCA-PSV 1.5 MoMs for gestational age is consistent with absence of moderate to severe anemia.
MCA MCA Use in FGR follow up The MCA PI can be the first parameter to become abnormal in late FGR ( 20% ) and associated with a higher incidence of suboptimal neurodevelopmental outcome at two years of age compared with a normal MCA PI
Ductus Ductus venosus venosus
Ductus Ductus venosus venosus Doppler Doppler Normal flow in the fetal ductus venous (DV) is forward and uniform . With progressively increasing UA resistance in FGR, fetal cardiac performance becomes impaired and atrial pressure increases, resulting in reduced diastolic flow in the DV a-wave. With progression of the severity of FGR, and late in the course of the disorder, the a-wave becomes absent or reversed
Other Doppler Other Doppler index for predicting index for predicting perinatal outcome outcome perinatal Cerebroplacental ratio The cerebroplacental ratio (CPR) is the MCA PI divided by UA PI . The CPR reflects both the placental status and fetal response and thus may be a sensitive Doppler index for predicting perinatal outcome . In late-onset FGR,the clinical value of this ratio has not been established, (CPR <1, <1.05, 1.08, <5thpercentile) More data are needed to determine whether CPR should be used in clinical practice to monitor FGR. Umbilicocerebral ratio The umbilicocerebral ratio (UCR) is the MCA PI divided by UA PI. abnormal UCR (defined as >0.8) The UCR may allow for better differentiation of Doppler abnormalities than the CPR; however, the clinical value of this ratio has not been established.
Uterine artery Doppler study Uterine artery Doppler study
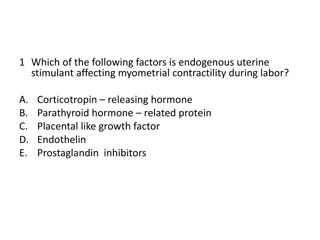
1) Prediction of preeclampsia 1) Prediction of preeclampsia Two types of uterine artery Doppler waveform analysis techniques : (1) presence or absence of diastolic notching (unilateral, bilateral) of the uterine arcuate vessels and (2) flow waveform ratios (eg, high resistance or pulsatility index, systolic/diastolic ratio).
prediction of preeclampsia prediction of preeclampsia Uterine artery Doppler ultrasonography was more accurate for prediction of preeclampsia when performed in the second trimester than in the first trimester. the overall risk of preeclampsia was best predicted by second-trimester elevation of pulsatility index accompanied by uterine artery notching
2) Prediction of FGR 2) Prediction of FGR Uterine artery Doppler ultrasonography in the second trimester second-trimester elevation of pulsatility index uterine artery notching
FGR definition FGR definition SMFM-ACOG-AIUM guiedlines : AC or EFW <10thcentile for GA SMFM: Society for Maternal-Fetal Medicine; ACOG: American College of Obstetricians and Gynecologists; AIUM: American Institute of Ultrasound in Medicine; ISUOG: International Society of Obstetricians and Gynecologists
diagnostic criteria for fetal growth diagnostic criteria for fetal growth restriction restriction ISUOG : Early (<32 weeks) AC or EFW <3rd centile for GA or UA-AEDF ISUOG : Late ( 32 weeks) AC or EFW <3rd centile for GA Or Or AC or EFW <10thcentile Combined with one of the following: UtA PI >95thcentile UA-PI >95thcentile Any two of the following: AC or EFW <10thcentile for GA AC/EFW crossing centiles >2 quartiles on growth centiles CPR <5thcentile or UA-PI >95thcentile
Fetal Fetal surveillance IN FGR surveillance IN FGR Estimated fetal weight (EFW): every 2-4 W Doppler ultrasonography UtA UA MCA DV Fetal behavior (biophysical profile [BPP] and nonstress test [NST]/cardiotocography [CTG])
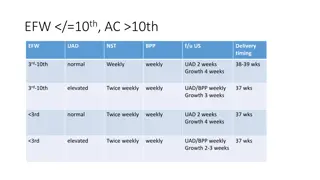
Doppler Doppler ultrasonography ultrasonography in FGR in FGR If the UA and MCA Doppler (if performed because of late-onset FGR) are normal (UA pulsatility index [PI] 95thand MCA PI 5thpercentile), UA and MCA Doppler and a BPP are performed at weekly intervals. If either the UA or MCA Doppler (if performed because of late-onset FGR) is abnormal but the UA has diastolic flow (UA PI >95thand MCA PI <5thpercentile), amniotic fluid volume is normal, and no concerning maternal or fetal comorbidities exist, UA and MCA Doppler are performed twice a week and a BPP is also performed at one of the visits and an NST is performed at the other visit. Patients with abnormal UA or MCA Doppler but UA diastolic flow and concerning comorbidities (eg, oligohydramnios, preeclampsia, chronic hypertension) admitted to the hospital. Following 24-hour inpatient observation and fetal monitoring, care is individualized (inpatient versus outpatient monitoring versus delivery).
Doppler Doppler ultrasonography ultrasonography in FGR in FGR If the UA Doppler has absent or reversed diastolic flow, admitted (frequent fetal surveillance and to enable prompt fetal evaluation in the event of decreased fetal activity or other pregnancy complications.) NSTs are performed every 6 to 12 hours, a BPP is performed daily, UA and MCA Doppler are performed two to three times per week. DV Doppler. Absent or reversed DV a-wave (represents an advanced stage of fetal compromise and can be an additional factor to consider during counseling and shared decision-making) ; however, this finding alone is not an indication for delivery
DELIVERY in FGR DELIVERY in FGR Patients with a reactive NST and BPP score 8/8, 10/10 or 8/10 with normal amniotic fluid volume: UA reversed diastolic flow between 30+0 and 32+0 weeks of gestation or at diagnosis if diagnosed at >32+0 weeks. UA absent diastolic flow between 33+0 and 34+0 weeks of gestation or at diagnosis if diagnosed at >34+0 weeks. UA pulsatility index (PI) abnormal (PI >95thpercentile) at 37+0 weeks or at diagnosis if diagnosed at >37+0 weeks.
DELIVERY in FGR DELIVERY in FGR UA PI normal (PI 95thpercentile): -EFW <3rdpercentile and no comorbidities Deliver at 37+0 weeks or at diagnosis if diagnosed at >37+0 weeks. -EFW 3rdand <10thpercentile and no comorbidities Deliver between 38+0 and 39+0 weeks of gestation or at diagnosis if diagnosed at >39+0 weeks. -FGR with oligohydramnios or comorbidities (eg, preeclampsia, chronic hypertension) Timing should be individualized, but most patients should be delivered between 34+0 and 37+6 weeks of gestation
Preeclampsia Preeclampsia Assessment of fetal well-being twice weekly nonstress testing (NST) plus amniotic fluid volume Or twice weekly biophysical profiles (BPP) beginning at the time of preeclampsia diagnosis, and also suggest that patients perform daily fetal movement counts. Fetal testing (NST or BPP) should be performed promptly if there is an abrupt change in maternal condition or decreased fetal activity. Evaluation of umbilical artery Doppler velocimetry indices is useful if fetal growth restriction is suspected, as the results help to optimize delivery timing to prevent perinatal death
Polyhydramnios Polyhydramnios Criteria for mild, moderate, and severe polyhydramnios Doppler study : Measure middle cerebral artery (MCA) post systolic velocity (PSV) : MCA-PSV performs well from 25 to 35 weeks of gestation.Doppler findings suggestive of moderate and severe fetal anemia (MCA-PSV 1.5 multiples of the median [MoM]) Mild SPD : 8.0 to 11.9 cm AFI :24.0 to 29.9 cm Moderate : SPD :12.0 to 15.9 cm AFI : 30.0 to 34.9 cm Severe SPD : 16.0 cm AFI : 35.0 cm
Oligohydramnios Oligohydramnios Diagnosis The diagnosis is based on any of the following: Amniotic fluid index (AFI) 5 cm Single deepest pocket (SDP) <2 cm Doppler velocimetry is only used to monitor pregnancies with FGR
Twin pregnancy Twin pregnancy
Twin pregnancy Twin pregnancy
Twin pregnancy Twin pregnancy
Twin pregnancy Twin pregnancy