Improving Bedside Shift Report Behavior on Medical-Surgical Unit
Explore the importance of enhancing bedside shift report behavior to address patient safety risks and improve communication effectiveness. Learn about the impact of ineffective nursing handoff communication, patient harm, and associated costs. Discover microsystem assessments, patient satisfaction scores, cost analysis due to communication errors, and qualitative costs on staff perceptions and satisfaction.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
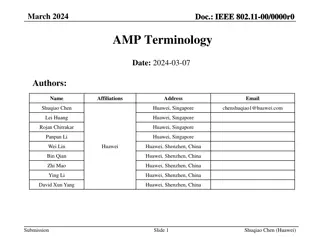
Improving the Quality of Bedside Shift Report Behavior on Improving the Quality of Bedside Shift Report Behavior on the Medical the Medical- -Surgical Unit at Woodland Healthcare Surgical Unit at Woodland Healthcare Amanda Waggoner, RN, MSN
Purpose Ineffective nursing handoff communication at shift change Delay in or inappropriate treatment Extended LOS Increased preventable costs Decreased patient and staff satisfaction Patient harm Leading cause of sentinel events Importance of addressing patient safety risks as a priority https://www.google.com/search?q=communication+errors+between+nursese&tbm=isch&tbs=rimg:CfjHKqO1bX_1FIjh_1xReqCT1ILjX4Tdmgvg2tjBtocqK6RZ1plxlwjX-
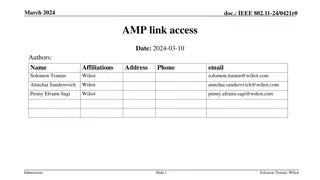
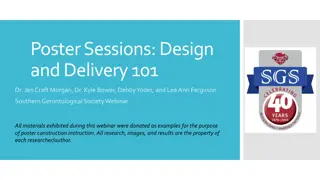
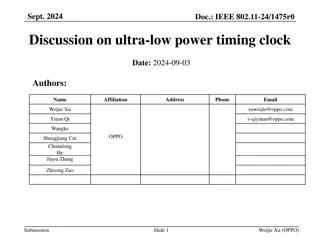
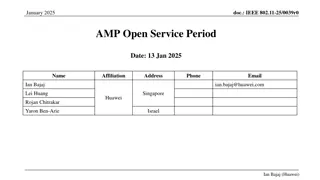
Microsystem Assessment 5P s Assessment Process Identification Observation of BSR Communication Assess quality report at bedside Began on time, introduction, information exchange (SBAR), patient involvement, Safety San. Lack of BSR altogether Nursing Satisfaction Survey Only 40% of day shift Nurses felt satisfied with shift report 50% of night shift felt report time is adequate BSR performance of twenty 12 hour night shift RNs 20 15 10 10 10 6 5 0 BSR Did not perform BSR performed
Microsystem Assessment Press Ganey Scores At shift change, do patient s feel included in the plan of care? Yes; Total Mean= 89.3 July 03, 2017 Sex 59% Females, 41 % Males Language- 89% English, 11% Spanish Reportable Events Kinked Foley Patient Fall Hypoglycemic Episode https://myhealth.alberta.ca/alberta/pages/When-you-have-an-indwelling-catheter-after-your-visit.aspx
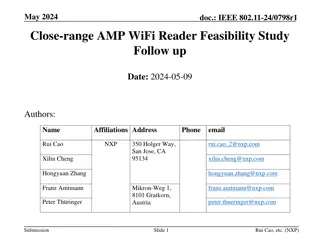
Kinked Foley= $4,500 Lab Testing Extended LOS x1 day Patient Fall= $5,200 X-ray of hip PT evaluation Pain medication Extended LOS x1 Hypoglycemic Episode= $13,300 Lab Testing Hypoglycemic management/ medications Extended LOS x3 days Cost Analysis $0 to implement BSR Total of $23,000 absorbed costs by the organization as a result of poor handoff communication related errors https://health.clevelandclinic.org/2012/11/healthcare-costs-and-you/
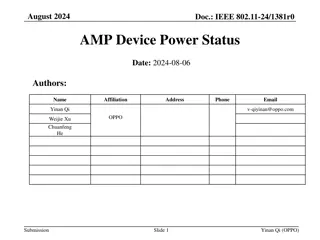
Qualitative Costs Daily living Staff perceptions Emotional Pain/ Suffering Physical Pain Patient/Staff Satisfaction Scores Financial Responsibilities Teamwork/ Communication/ Unit morale Relationship Strain https://archive.ahrq.gov/news/newsletters/research-activities/14jan/0114RA9.html
Literature Review PICO Strategy P: Medical-surgical nursing I: Bedside report tool C: Non-bedside shift report O: Effective communication at shift change as evidenced by improved patient outcomes, prevention of events, and improved patient and staff satisfaction. Benefits of BSR tool Clarification of significant information Physical examination of patient and environment/ safety checks Improved nursing accountability/ teamwork Improved patient and staff satisfaction Reduction of hand-off related errors (Ferguson & Howell, 2015)(Zou & Zhang, 2016)
Preparation Oncoming RN arrives on time to prepare for report. This means before 0700 or 1900 Report begins at 0700 or 1900. Introduction Off going nurse uses AIDET (Acknowledge, Introduce, Duration, Explanation, and Thank You) to introduce oncoming nurse to patient and family Update Whiteboards with correct information o Other team members may be present (CNAs, RT, Lab, etc). Information Exchange Use of SBAR (Situation, Background, Assessment, and Recommendation) Use of simple terms and language that patient and family will understand (including use of interpreter services as needed), avoid using medical terms that patient is unfamiliar with (i.e. NPO). WOW (Workstation on Wheels) present during bedside report utilized to clarify any information. Patient Involvement Give patient and/or family the opportunity to ask questions related to care, clarify exchanged information, review plan of care/ goals for the day including expected hourly rounding. Safety Scan Review the patient, environment, AND EHR (Electronic Health Record) bedside. o Patient Assessment: Visually inspect any and all incisions, wounds, .dressings, drains, catheters, IV lines. o Environment Assessment: Visually inspect IV pumps, oxygen, bed alarms, suction equipment, fall mats, call light and personal belongings within reach. Make sure bed is low and locked in position. o EHR: Review of medication administration record to verify all medications have been given and documented correctly, vital signs, I&Os, etc.
Specific Aim Statement Through implementation of a standardized bedside report tool, 95% of twelve-hour night shift nurses on the medical surgical unit at Woodland Healthcare will demonstrate proper quality bedside report at shift change by August 15, 2017.
Methodology Lewin s Theory of Planned Change Unfreezing: Presented evidence-based research during huddles, gained stakeholder interests, addressed staff barriers, provided education to staff. Moving: Monitored and coached staff during BSR. Act as resource for support/ mentoring. Refreezing: evaluate BSR utilizing competency checklist, post-implementation survey results of staff and patients. Enact sustainability plan.
Identification of Barriers Pre-Implementation Survey Nursing Survey Results Time constraints Nursing attitude/compliance HIPPA violations Language barrier Patient compliance
Timeline Gantt Chart
Summary Report Evaluation of Outcomes In the process of collecting post- implementation data and evaluating outcomes: Nursing Competency Checklist Press Ganey Survey Nursing post-implementation survey Review of reportable events What I learned The importance of flexibility and networking Setting realistic goals and objectives Utilizing effective communication strategies Application of the PDSA cycle
PDSA PDSA PDSS Aligning with WHC Mission and Vision -Dignity, collaboration, stewardship, justice, and excellence Having a unit champion - Key player and influencer Continued perceived benefits for staff and patients - Post results of improvement, storytelling Maintaining stakeholder support -Running reports and audits, benchmarking Sustainability Plan http://www.opendoorhr.com/Quality-Improvement-Process/
References Ferguson, T.D. & Howell, T.L. (2015). Bedside reporting protocols for improving patient care. Nursing Clinics of North America, 50(4), 735-747. Image one. (2017). Retrieved from https://www.google.com/search?q=communication+errors+between+nursese&tbm=isch&tbs=rimg:CfjHKqO1bX_1FIjh_1xReqCT1ILjX4Tdmgvg2tjBtocqK6RZ1plxlwjX- Image two. (2017). Retrieved from https://myhealth.alberta.ca/alberta/pages/When-you-have-an-indwelling-catheter-after-your-visit.aspx Image three. (2017) Retrieved from https://health.clevelandclinic.org/2012/11/healthcare-costs-and-you/ Image four. (2017). Retrieved from https://archive.ahrq.gov/news/newsletters/research-activities/14jan/0114RA9.html Image five. (2017). Retrieved from http://www.opendoorhr.com/Quality-Improvement-Process/ Zou, X.J. & Zhang, Y.P. (2016). Rates of nursing errors and handoffs-related errors in a medical unit following implementation of a standardized nursing handoff form. Journal of Nursing Care Quality, 31(1), 61-67.