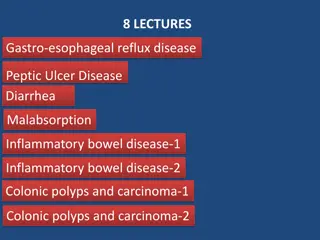
Malabsorption Syndromes Including Celiac Disease
Explore the various aspects of malabsorption syndromes, including Celiac disease, mechanisms of nutrient malabsorption, common causes, and treatment options. Learn about diarrhea, its categories, causes, and implications on intestinal fluid balance. Understand the distinction between maldigestion and malabsorption in nutrient absorption.
Uploaded on | 4 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Malabsorption Syndromes Including Celiac Disease
Objectives At the end of this presentation, students should: Understand the mechanisms of malabsorption of fats, carbohydrates, and proteins in common malabsorptive conditions Understand and be able to recognize some of the most common causes of nutrient malabsorption Know the options for treatment of common causes of malabsorption
Fluid Entering and Exiting the GI Tract Volume entering Volume absorbed 10 Duodenum and Jejunum (4) 8 Diet (2) Volume (L/day) Saliva (1) 6 Stomach (2) Ileum (3.5) 4 Bile (1) Volume Excreted 100-200 ml Pancreas (1) 2 S.I. (2) Colon (1.4) 0
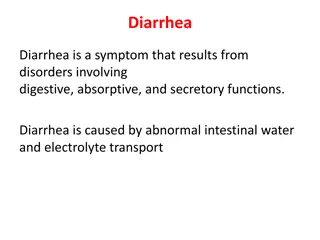
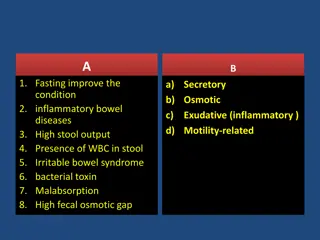
Diarrhea An increase in the frequency or decrease in the consistency of stools Results from an imbalance of intestinal fluid secretion and absorption Increased fluid secretion may overwhelm the ability of the small intestine and colon to absorb it Any significant decrease in fluid absorption can produce diarrhea even if fluid secretion remains constant Includes increased motility
Diarrhea Can be divided (roughly) into two categories Secretory Osmotic
Diarrhea Secretory diarrhea Results from increased fluid and electrolyte secretion (leakage) into the bowel lumen Example: cholera Osmotic diarrhea Results from decreased ability of the gut to absorb fluid Typically results from increased osmolarity of the luminal fluid caused by increased solute load Example: malabsorption, most laxatives Some conditions can have features of both Inflammatory bowel disease
Malabsorption Can be defined as diminished intestinal absorption of nutrients Can be helpful to distinguish between two processes Maldigestion Impaired ability to break macronutrients into absorbable monomers and oligomers Malabsorption Impaired ability to absorb digested nutrients across the intestinal epithelial mucosa
Malabsorption Can involve any nutrients Carbohydrate Fat Protein Micronutrients (vitamins, minerals) Can also involve bile acids Can be specific for one group of nutrients or affect multiple or all nutrients
Fat malabsorption Because of the complexity, fat digestion and absorption is the most common to be dysfunctional Problems can arise at any step of the process of digestion and absorption
Digestive Phase Absorptive Phase Pancreatic insufficiency Bile acid deficiency Celiac disease, Crohn s abetalipoproteinemia Intestinal lymphangiectasia
Phases of fat digestion Defects of lipolysis Anything that impairs the actions of lipase Deficiency of lipase (pancreatic insufficiency) Chronic pancreatitis Cystic fibrosis Inactivation of lipase (pH < 7) Zollinger-Ellison syndrome Chronic pancreatitis (decreased HCO3 secretion)
Phases of fat digestion Defects of micelle formation Bile acid deficiency
Bile acids Conjugated to glycine and taurine to give functional conjugated bile acids
Phases of fat digestion Defects of micelle formation Deficiency of bile acids Process Pathophysiologic defect Disease example Synthesis Decreased hepatic function Cirrhosis Biliary secretion Altered canalicular function Primary biliary cholangitis, obstructed common bile duct Maintenance of conjugated bile acids Bacterial overgrowth Jejunal diverticulosis, post- surgical anatomy Reabsorption Abnormal ileal function Crohn s disease, post- surgical anatomy
Phases of fat digestion Impaired migration into the epithelial cell Epithelial damage/disruption Celiac disease Crohn s disease Surgical alteration of anatomy Increased thickness of the unstirred water layer near the epithelial cells Bacterial overgrowth
Phases of fat digestion Impaired chylomicron formation Decreased (or absent) -lipoproteins Abetalipoproteinemia Impaired lymphatic drainage Damaged or absent lymphatic vessels Lymphatic obstruction Intestinal lymphangiectasia
Consequences If fats are not digested and absorbed, they remain in the lumen Steatorrhea Failure to absorb lipids results in loss of an important source of calories Also Loss of essential fatty acids Deficiency of fat-soluble vitamins (A, D, E, K)
Carbohydrate malabsorption Starches - amylase (saliva) pancreatic amylase Sucrose Lactose Maltose + 3-9 glucose polymers Sucrase Lactase Maltase + -dextinase Fructose Galactose Glucose
Carbohydrate malabsorption Carbohydrate malabsorption can be seen with pancreatic insufficiency, but is usually less significant than the fat malabsorption It can also be seen with widespread epithelial injury (severe Crohn s, celiac disease)
Carbohydrate malabsorption The only major carbohydrate malabsorption is lactase deficiency Usually acquired Common in all populations except Northern Europe and Caucasian Americans Results in lactose intolerance Abdominal cramping, diarrhea, flatulence after consuming lactose- containing foods Not all patients with decreased lactase have symptoms Treatment is elimination of dietary lactose Or use supplemental lactase Transient lactase deficiency is common after any gastroenteritis
Protein malabsorption Protein Pepsin Pancreatic proteases Di- and Tri-peptides Large peptides Free amino acids Carriers Peptidases Carriers Small amounts Dipeptides and tripeptides Amino acids Cytoplasmic peptidases Amino acids
Protein malabsorption Protein malabsorption can be a component of any generalized intestinal epithelial injury Severe Crohn s Celiac Can also be seen with pancreatic insufficiency In these conditions, it is usually overshadowed by malabsorption of other nutrients Isolated or selective protein malabsorption is rare
Protein-losing enteropathy More commonly-encountered clinical entity Results from chronic loss of protein due to leakage of protein into the intestinal lumen Can be seen with chronic diseases involving the GI tract
Protein-losing enteropathy Inflammatory/ulcerative diseases Crohn s/ulcerative colitis Celiac disease Peptic ulcer disease GI Carcinomas Disorders of lymphatic obstruction Malignant obstruction Intestinal lymphangiectasia Congestive heart failure
Protein-losing enteropathy Results in generalized protein deficiency, similar to nephrotic syndrome Albumin Immunoglobulins May also lose lymphocytes If lymphatics are obstructed Diagnosis Fecal alpha-1 antitrypsin level Not normally found in stool Resistant to degradation by digestive enzymes
Specific disease states Celiac disease Crohn s disease Pancreatic insufficiency Short-bowel syndrome Small intestinal bacterial overgrowth Post-bariatric surgery
Celiac disease Inflammatory condition, primarily of the small intestine, caused by immune stimulation by dietary gluten Results in immune-mediated damage to the small intestinal epithelium, resulting in dysfunction Can result in malabsorption of one or multiple nutrients Can be macro- or micronutrients or electrolytes No specific pattern
Celiac disease Manifestations Can cause diarrhea and weight loss due to malabsorption Can cause symptoms or lab findings of nutrient malabsorption Anemia Hypoalbuminemia Edema Iron/folate deficiency Osteomalacia Other vitamin deficiencies Electrolyte disturbances May cause nonspecific symptoms Fatigue, headache, malaise
Celiac disease Confirmatory diagnosis is by endoscopic biopsy of the small bowel Typically duodenum Very good serologic tests are available Anti-tissue transglutaminase (tTG) antibodies Anti-endomysial antibodies IgA High sensitivity and specificity Treatment is dietary elimination of gluten- containing foods Wheat, rye, barley, oats
Crohns disease Chronic inflammatory disease of the GI tract Causes segmental inflammation which can affect the entire thickness of the gut wall Fistulas Strictures Can occur in any area of the GI tract With widespread involvement of small bowel, can have malabsorption Especially if combined with prior surgical resections You will learn more about this in the TBL.
Pancreatic insufficiency Chronic injury to the pancreas can result in severe impairment of exocrine pancreatic function Chronic pancreatitis Cystic fibrosis With 90-95% of pancreatic exocrine function loss, malabsorption becomes clinically evident Steatorrhea Weight loss Supplemental pancreatic enzymes are used to help restore some normal digestion You will learn more about this in the other TBL.
Short bowel syndrome Results from surgical resection of a large portion of the small intestine Trauma Crohn s Postoperative scarring Mesenteric vascular disease Neonatal Congenital malformations Omphalocele Gastroschisis Necrotizing enterocolitis Can also result from rare congential intestinal disorders Microvillus inclusion disease
Short bowel syndrome Results from inadequate mucosal surface area to perform adequate absorption Typical symptoms are diarrhea and weight loss Following intestinal surgery, some adaptation may occur May take 6-12 months If enough bowel is removed, adequate adaptation cannot occur
Short bowel syndrome Management involves nutritional support Parenteral nutrition Maintain oral intake as well Must also observe for other complications Bile salt diarrhea (if distal ileum resected) Kidney stones (oxalate stones) Cholesterol gallstones
Small intestinal bacterial overgrowth Proliferation of bacteria in the small intestine Typically coliforms Due to alterations of the small bowel Function (stasis) Anatomy (postoperative) Diameter (short bowel) Manifestations Diarrhea Malabsorption +/- bacterial toxins Steatorrhea Impaired micelle formation and absorption Anemia (macrocytic) B12 depletion
Small intestinal bacterial overgrowth Diagnosis Hydrogen breath test Quantitative small bowel culture Clinical suspicion Treatment Cycled antibiotics
Post-bariatric surgery Malabsorption is intentional following bariatric surgery Can be greater than intended Deficiencies of micronutrients are very common following some bariatric procedures
Post-bariatric surgery Manifestations may include Weight loss Anemia (Fe, folate) Edema (protein malabsorption) Neuropathy (thiamine, copper) Impaired wound healing (zinc, vitamin A) Osteomalacia (vitamin D) Typically, patients who have had malabsorptive procedures should have monitoring of micronutrient levels and common lab parameters following surgery If manifestations become severe, reversal of the surgery may be required
Approach to patients Suspect malabsorption when patients report Diarrhea with weight loss Oil droplets or fat in stools Diarrhea that resolves with fasting History of conditions associated with malabsorption (prior pancreatitis, Crohn s, etc) Diagnosis of malabsorption Fecal fat testing Check levels of fat-soluble vitamins Look for specific causes