Understanding Meningococcal Disease: Causes, Symptoms, and Treatment
Meningococcal disease, caused by Neisseria meningitidis, is a serious and potentially life-threatening illness affecting mainly children and young adults. This article provides insights into the historical perspective, epidemiology, and characteristics of the bacteria responsible for meningococcal meningitis. Learn about the alarming mortality rates, prevalent serotypes, and the global impact of this disease.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Meningococcemia and Meningococcal Meningitis
Meningococcus Meningococcal disease is a frightening illness. Generally attacks young healthy individuals. Patients can go from well to death in 24 hours. The combination of meningitis and endotoxemia makes it a double life threatening disease. It can cause large outbreaks or sporadic cases.
Meningococcal Disease Worldwide: there are ~ 500,000-1,200,000 cases of invasive disease per year. 50,000 135,000 deaths per year. Second most common cause of bacterial meningitis, in those over 2 years of age. children account for majority of cases. In the US, meningococcus is the most common cause of meningitis in adolescents and young adults, and the second most common cause in adults. Overall mortality rate of meningococcal meningitis is ~10-15% in the US for sporadic disease. Higher in 16-25 yo (25%) vs <15 yo.
Historical Perspective Incredibly, the first description of meningococcal meningitis was not made until 1805, by Viesseux, who called it purpuric meningitis. This implies that a change in the virulence for humans occurred early in 1800 s for this pathogen. During the decades prior to the beginning of the antibiotic era, mortality was close to 80%. Treatment consisted of systemic and intrathecal injection of meningococcal antisera from horses.
The Bug: Neisseria meningitidis Gram-negative diplococcus (kidney shaped). capsule: all invasive isolates are encapsulated. Very fastidious should be processed quickly, as it is very sensitive to drying, cold and high pH. Chocolate Agar or Thayer Martin. Many Serotypes, based on capsular polysacchs: most common causes of human disease are A, B, C, Y, and W- 135. A, B and C cause 90% of all human disease (WHO). Y has gained imp. in US. B causes most infant cases. In sub-Saharan Africa, explosive outbreaks have been reported, mostly with A and C.
Epidemiology Epidemic and Sporadic forms of disease. Most common in the dry season/winter months, when low humidity may alter the pharyngeal mucosal barrier, predisposing it to infection. Mostly affects children and young adults. In the US, children <5 account for 55% of cases. During epidemics, increased rates occur in older populations. Increased incidence in males, may be skewed by outbreaks in military recruits and alcoholics. Rates increasing in elderly. Highest incidences are seen in the meningococcal belt of sub- Saharan Africa, and in Saudi Arabia (Mecca) during Haj. Outbreaks occur in sub-Saharan Africa (usually A and C) every 7-10 years, with case rates as high as 1/1000 population (1/100 children 0 2 yo).
Episodic and Epidemic Nature Outbreaks occur in both developed and developing countries. All serogroups can cause epidemics, although they differ in epidemiology and rates of attack. A and C are more common in developing countries, with very high attack rates (500/100,000). B is common in developed countries and has lower attack rates (50/100,000). It is the most common cause of sporadic infection in the US. There is a close relationship between carriage rate and the rise and fall of an epidemic. Transmission from one carrier to another, is via the respiratory droplets.
Risk Factors during Epidemics Nasopharyngeal carriage with encapsulated isolates. Crowding and lower socioeconomic status. Poor general health. Alcoholism. Terminal complement deficiency. Eculizumab use for HUS or PNH monoclonal Ab aimed at terminal complement. Asplenia or hyposplenia. HIV/AIDS.
MSM / HIV Outbreak in NYC 2013. Social media. Led to vaccination of all HIV positive patients in NYC and nationwide. Strain was serotype C. Similar outbreaks reported in Europe.
Nasopharyngeal Colonization NP colonization is a pre-requisite for invasive disease. Meaning, the NP is the portal of entry. Transmission is via aerosol droplets. Neisseria attach to epithelial cells using adhesion proteins. Less than 1/1000 colonized patients develop invasive disease, possibly because many carriers (up to 90%) are colonized with non-encapsulated (non-typable) isolates. As little as 20% of military recruits carry the organism within 7 days of hospitalization. Implying that invasive disease is often due to very recent infection.
Immunity Disease risk is inversely related to the development of bactericidal anti-meningococcal capsular antibodies. Pharyngeal colonization may elicit the development of these antibodies. The capsule is antiphagocytic and anti-complement lysis. During one outbreak in army recruits in 1968, the sera of 5.6% of infected recruits contained bactericidal antibodies (bactericidal defect), versus 82.2% of controls. Complement plays an important role; patients with isolated deficiencies of late complement components, are at increased risk of recurrent Neisseria infections. Recovery from invasive disease does not confer lifelong immunity. Patients with complement deficiency can get illness recurrences, though usually they are milder.
Pathogenesis of N. meningitidis Colonization of the oropharynx with an encapsulated isolate. Local invasion, if conditions are ripe. Bacteremia. Invasion into subarachnoid space. Meningeal inflammation, leading to the symptoms and complication of meningitis.
Meningococcus Spectrum of Disease 1) Bacteremia without sepsis: patient presents with upper respiratory tract infection and has bacteremia which is clinically inapparent. 2) Meningococcemia without meningitis: sepsis syndrome, with classic features of endotoxemic state, including DIC and shock. 3) Meningitis with or without meningococcemia: Clinical case of meningitis, with or without the sepsis syndrome of meningococcemia.
Clinical Manifestation 1) Meningeal Related to meningeal irritation by pathogen. 2) Meningococcemia related to sepsis, and due to the release of endotoxin into the brain and blood stream.
Clinical Manifestations As mentioned, patient go from healthy to critically ill and even death within hours. Patients will often say they ve never been this sick. Sudden onset of fever, headache, myalgias, often with nausea, vomiting, loss of appetite, pharyngeal pain. Myalgias can be quite severe. Patients often lack the classic triad of fever, stiff neck and altered MS (pneumococcus), but the petechial rash makes diagnosis more likely. Altered mental status, petechial rash and stiff neck are often late manifestations, so high index of suspicion is needed before the rash is present.
Clinical Manifestations Meningeal Headache, nuchal rigidity, nausea, vomiting, photophobia, altered mental status. These symptoms may be less evident in the very young and elderly. Focal neurologic symptoms and seizures may be less common than with pneumococcus. Kernig sign: place patient in supine position with hips at 90 deg angle and then extend the knee. Positive if there is resistance to extension or pain. Brudzinski sign: place patient in supine position and flex head towards chest. Positive if hips/knees flex.
Clinical Manifestations Meningococcemia Associated with endotoxemia (LOS). Shock! Early shock: leg pain, cold hands/feet and pallor or mottling of skin median 8 hours into Sx onset. Hypotension, tachycardia, acidosis, DIC, altered mentation, hypoxia, cyanosis, adrenal failure. Rash: petechiae due to DIC (50% at presentation). Most frequently on palpebral conjunctiva, mucosa and trunk. May coalesce or cluster. Purpura Fulminans (severe). Waterhouse-Friderichsen Syndrome: due to hemorrhage or infarction, leading to adrenal failure, vascular collapse, multi-organ damage, and death. Cardiac complications: myocarditis and cardiac failure due to shock. Associated with increased mortality.
Lipo-oligosaccharide (Endotoxin) Lipo-oligosaccharide (LOS) is an antigen of the meningococcal outer membrane. It is similar to LPS of other gram-negative bacteria. LPS is a potent activator of pro-inflammatory cytokines, particularly TNF- . Does this by mimicking human tissue antigens, allowing it to interact with human cells (macrophages, PMNs, endothelial cells), and cause the release of cytokines. Highest levels of endotoxin seen in any human disease. High levels of free TNF- in plasma have been associated with increased morbidity and mortality in patients with meningococcemia.
Lipo-oligosaccharide (Endotoxin) When LPS comes into contact with APC s, there is a rapid and excessive production of cytokines: TNF- , IL- 1, IFN- , and colony stimulating factors. These trigger the activation of the complement, clotting, fibrinolytic, and kinin pathways, as well as other pro- inflammatory factors. Effects on tissue metabolism, cardiac function, and vascular tone, lead to the damage seen. End-organ damage results from tissue hypoxia. Clinical features: fever, edema, DIC, hypotension, and cardiac failure (myocarditis).
Diagnosis and Work-up Assess the patient for features of meningitis headache, photophobia, neck stiffness, irritability, altered mental status. In children, check for Kernig and Brudzinski signs meningeal irritation. Full body exam looking for petechiae. Monitor vitals closely tachycardia, mild hypotension may be early sign of shock. Cyanosis, pallor, cold extremities. Rapid work up is essential!! It is critical to note that if you consider meningococcal disease, you must administer antibiotics immediately (after blood cultures are drawn w/o delay)
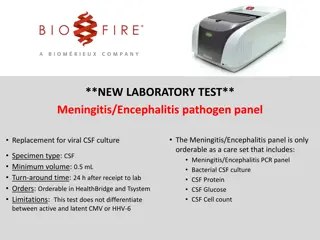
Diagnosis and Work-up If you suspect meningococcal invasive disease: Draw BCx s immediately, then initiate antibiotics without delay 50-60% will have positive BCx s. Don t wait for an LP (or a head CT) to start antibiotics, or the patient will die!! CSF: very high WBC (polys), high protein, low glucose. Opening pressure may be elevated, if ICP is high. Gram stain should be done in all patients, esp if abx given. Gives immediate diagnosis. 80-90% will have positive culture if no abx given. Sterilization of CSF occurs within 1-2 hours of abx administration. PCR will remain positive despite abx use. Sens/Spec: 96/100%
Empiric Treatment Again, any patient presenting with fever, severe sepsis, petechiae, or suspected meningitis, should receive immediate broad antimicrobial therapy. Initial Empiric therapy for bacterial meningitis: Vanco / CTX / Decadron, +/-Ampicillin (for Listeria), +/- Rifampin. Strep pneumo, N meningitides, Listeria (usually preg or >50) Children <1 month may also have, GBS, E coli and Listeria. Children 1 month to 2 years can have all of the above. If OP or Rural setting 2 gm IM CTX prior to transport should be given if available and won t significant delay transport. If CSF culture is negative, but clinical picture and CSF fit, complete course for bacterial meningitis.
Specific Therapy for Meningococcus Ceftriaxone (or Cefotaxime) is the drugs of choice. CTX 2 gm every 12 hours for 7 days. Beta lactamase containing Meningococci remain susceptible to CTX but not to penicillin (up to 25% in some locations). In one French study, 2% of isolates had reduced susc to CTX (worrying). Chloramphenicol / Meropenem / Aztreonam / FQ for CTX resistance. If PCN susceptible (MIC <0.1), then PCN 4 mu q4 may be used. PCN will not eradicate NP colonization. If severe allergy to B lactams Chloramphenicol , aztreonam or FQ. Duration: 4-7 days. I use 7 days in everyone. Supportive care for shock and other complications.
Dexamethasone use ~25% of patients with Menigococcal meningitis will have some form of neurologic sequelae: hearing loss, seizure, learning disability, headache, visual defects. Dexamethasone has been shown to prevent sequelae in HIB and in Pneumococcal meningitis, but 2002 study was not powered for Neisseria (much fewer cases). Hearing loss, neurologic complication (seizure) and mortality. Should be given before or at abx initiation. Not after! Dose: 0.15 mg/kg q6 hours for 4 days. There is controversy around it s use in Meningococcal meningitis. Empirically, all patients with presumed bacterial meningitis should get it. Once Pneumococcus ruled out, most authorities recommend discontinuation.
Mortality Mortality today is 10-15% despite antibiotic use. Causes of death are usually due to: 1. Cerebral edema: leading to damage to vital areas of the brain, particularly in the midbrain. This is caused be meningeal inflammation, which is due to the inflammatory cell of the immune response and to endotoxin release in the CSF. 2. Septic shock: due to endotoxin release in the CSF and systemic circulation, causing cytokine release, hypotension and DIC (bleeding). Shock may also be caused by bleeding into the adrenal glands, leading to adrenal failure
Prevention - Chemoprophylaxis Chemoprophylaxis: Used to eliminate carriage during epidemics and sporadic infection. Given to all close contacts: all family members, nursery school or dorms or barracks contacts, and those with contact with secretions of source patient. Rifampin (4 doses), Cipro, Ceftriaxone (single doses). Follow-up of 10 days if presenting after 10 days of exposure no need to treat.
Prevention - Vaccination Two vaccines available: Quadrivalent (A, C, Y, W-135) vaccines and Monovalent vaccines (A, B and C), though B is most important. Who should get them: Main target population: adolescents, prior to high risk at 11-12 yo and booster prior to college or Army (immunity wanes). Military recruits and first year college students if not vaccinated prior. Immunocompromised: C50 def, asplenic, HIV/AIDS, C5 inhib. Booster as needed. Microbiologists, living in endemic area, during outbreak. Introduction of vaccination has decreased rates of meningitis and increase age of cases. (Same for HIB/Pneumoccocus)