Understanding Plasma Proteins and Their Functions
Plasma proteins play a crucial role in various physiological functions such as controlling extracellular fluid distribution and transportation of hormones, vitamins, and other substances. The balance between protein synthesis and catabolism determines protein levels in the vascular compartment, affecting overall health. Qualitative methods like electrophoresis help in studying plasma proteins. Understanding the distribution and functions of these proteins is essential for maintaining proper bodily functions.
Understanding Plasma Proteins and Their Functions
PowerPoint presentation about 'Understanding Plasma Proteins and Their Functions'. This presentation describes the topic on Plasma proteins play a crucial role in various physiological functions such as controlling extracellular fluid distribution and transportation of hormones, vitamins, and other substances. The balance between protein synthesis and catabolism determines protein levels in the vascular compartment, affecting overall health. Qualitative methods like electrophoresis help in studying plasma proteins. Understanding the distribution and functions of these proteins is essential for maintaining proper bodily functions.. Download this presentation absolutely free.
Presentation Transcript
PLASMA PROTEINS The amount of protein in the vascular compartment depends on the balance between the rates of synthesis and catabolism or loss. However, also important is the relative distribution between the intravascular and extravascular compartments, as the concentration depends on the relative amounts of protein and water in the vascular compartment. Therefore, abnormal concentrations do not necessarily reflect defects in protein metabolism
Protein synthesis Hepatocytes synthesize many plasma proteins; those of the complement system are also made by macrophages. Immunoglobulins are mainly derived from the B lymphocytes of the immune system. Protein catabolism and loss Most plasma proteins are taken up by pinocytosis into capillary endothelial cells or mononuclear phagocytes, where they are catabolized. Small-molecular-weight proteins are lost passively through the renal glomeruli and intestinal wall. Some are reabsorbed, either directly by renal tubular cells or after digestion in the intestinal lumen; others are catabolized by renal tubular cells
Function of plasma protein 1-Control of extracellular fluid distribution The distribution of water between the intravascular and extravascular compartments is influenced by the colloid osmotic effect of plasma proteins, predominantly albumin 2-Transport function Albumin and specific binding proteins transport hormones, vitamins, lipids, bilirubin, calcium, trace metals and drugs. Combination with protein allows poorly water-soluble substances to be transported in plasma. The protein-bound fraction of many of these substances is physiologically inactive, unlike the unbound fraction.
Qualitative methods for studying plasma and urinary proteins Electrophoresis Electrophoresis is a technique that separates compounds such as proteins according to their different electrical charges. It is usually performed by applying a small amount of serum to a strip of cellulose acetate or agarose and passing a current across it for a standard time. In this way, five main groups of proteins namely albumin and the 1, 2, and g globulins may be distinguished after protein staining and may be visually compared with those in a normal control serum. The following description applies to the normal appearance, in adults, of the principal bands seen after electrophoresis on cellulose acetate:
Albumin, usually a single protein, makes up the most obvious band. alpha1-globulins consist almost entirely of alpha1-antitrypsin and alpha1-antichymotrypsin. alpha2-globulins consist mainly of alpha2-macroglobulin and and haptoglobin -globulins often separate into two; 1 consists mainly of transferrin and lipoprotein (LDL), and 2 consists of the C3 (component of complement.) g-globulins are immunoglobulins; some immunoglobulins are also found in the alpha2 and regions. If plasma rather than serum is used, fibrinogen appears as a distinct band in the g region.
Electrophoretic patterns in disease Parallel changes in all protein fractions Reduction may occur in severe undernutrition, sometimes due to malabsorption, unless accompanied by infection and haemodilution. An increase may occur in haemoconcentration. The acute-phase pattern Tissue damage usually triggers the sequence of biochemical and cellular events associated with inflammation. The biochemical changes include the stimulation of synthesis of the so-called acute-phase proteins, with a rise in the alpha1-globulin and alpha2-globulin fractions. The plasma concentrations of these proteins reflect the activity of the inflammatory response, and their presence is responsible for the rise in the erythrocyte sedimentation rate (ESR) and increased plasma viscosity characteristic of such a response.
Chronic inflammatory states In chronic inflammation, the usual increase in immunoglobulin synthesis may be visible as a diffuse rise in g-globulin. If there is an active inflammatory reaction , the increased density in the g-globulin region is associated with an increase in the alpha1 and alpha2 fractions of the acute-phase response Cirrhosis of the liver The changes in the concentrations of plasma proteins usually are non-specific , but in cirrhosis a characteristic pattern is sometimes seen. Albumin and often alpha1- globulin concentrations are reduced and the g-globulin concentration is markedly raised, with apparent fusion or bridging of the b and g bands because of an increase in plasma IgA concentrations
Nephrotic syndrome Plasma protein changes depend on the severity of the renal lesion. In early cases, a low plasma albumin concentration may be the only abnormality, but the typical pattern in established cases is reduced albumin, alpha1-globulin and sometimes g-globulin bands and an increase in alpha2-globulin concentration due to a relative or absolute increase in the high-molecular-weight a2- macroglobulin. If the syndrome is due to conditions such as systemic lupus erythematosus (SLE), the g-globulin concentration may be normal or raised. a1-Antitrypsin deficiency The alpha1 band consists almost entirely of a1-antitrypsin and its absence or an obvious reduction in its density suggests a1-antitrypsin deficiency
Albumin Albumin, with a molecular weight of about 65 kDa, is synthesized by the liver. It has a normal plasma biological half-life of about 20 days. About 60 per cent in the extracellular fluid is in the interstitial compartment. However, the concentration of albumin in the smaller intravascular compartment is much higher because of the relative impermeability of the blood vessel wall. This concentration gradient across the capillary membrane is important in maintaining plasma volume
Cuases of hypoalbuminaemia Dilutional hypoalbuminaemia 1-Dilutional hypoalbuminaemia may, as in the case of total protein, result from artefactual changes due to taking blood from the arm into which an infusion is flowing, administration of an excess of protein-free fluid or fluid retention, usually in oedematous states or during late pregnancy. 2-Redistribution of albumin Redistribution of albumin from plasma into the interstitial fluid space results from: 1-Recumbency: plasma albumin concentrations may be 5 10 g/L lower in the recumbent than in the upright position because of the redistribution of fluid. 2-Increased capillary membrane permeability: this is the usual cause of the rapid fall in plasma concentration found in many circumstances, for example postoperatively and in most illnesses.
Decreased synthesis of albumin 1-undernutrition, resulting in an inadequate supply of dietary nitrogen, 2- malabsorption, resulting in impaired absorption of dietary peptides and amino acids, 3- impairment of synthesis, due to chronic liver dysfunction, for example cirrhosis Increased loss of albumin from the body 1-the skin, because of extensive burns or skin diseases such as psoriasis; a large part of the interstitial fluid is subcutaneous, 2-the intestinal wall, in protein-losing enteropathy, 3-the glomeruli, in the nephrotic syndrome. Increased catabolism of albumin Catabolism (and therefore nitrogen loss) is increased in many illnesses, including sepsis and hyperthyroidism.
Consequences of hypoalbuminaemiaThe following may occur. Fluid distribution Albumin is quantitatively the most important protein contributing to the plasma colloid osmotic pressure Oedema may occur in severe hypoalbuminaemia Binding functions Albumin binds calcium, bilirubin and free fatty acids.drugs
Paraproteinaemia The term paraprotein (or also called M protein) refers to the appearance of an abnormal, narrow, dense band on the electrophoretic strip. It is found most commonly in the g region, but may be anywhere from the alpha2 to the g region. Paraproteins can often be shown to be monoclonal. Causes of paraproteinaemia myelomatosis, which accounts for most of the cases of malignant paraproteinaemia macroglobulinaemia (Waldenstr m smacroglobulinemia) B-cell lymphomas, including chronic lymphatic leukemia,, sometimes in SLE, chronic inflammation or infections and cryoglobulinaemia
The consequences of malignant B-cell proliferation 1-increased plasma viscosity 2-A high plasma total protein concentration 3-Hyponatraemia 4-Bence Jones protein 5-normochromic normocytic anaemia, a common presenting feature of any malignant disease, 6- haemorrhages, perhaps due to complexing of coagulation factors by the paraprotein, 7- Raynaud s phenomenon, which may occur if the paraprotein is a cryoglobulin, 8-hypercalcaemia may also be present
Myelomatosis (multiple myeloma; plasma-cell myeloma) Myelomatosis is caused by the malignant proliferation of plasma cells throughout the the bone marrow. The condition becomes increasingly frequent after the age of 50; it can occur before the age of 30, but is rare. The sex incidence is about equal. The clinical features are due to malignant proliferation of plasma cells and disordered immunoglobulin synthesis and/or secretion from the cell. Bone pain may be severe and is due to pressure from the proliferating cells. Radiographs may show discrete punched-out areas of radiotranslucency in the skull, vertebrae, ribs and pelvis.
There may be generalized osteoporosis. Pathological fractures may occur. Histologically there is little osteoblastic activity around the lesion, which arises in the marrow rather than in the bone itself; consequently, the plasma alkaline phosphatase activity is normal unless there is liver involvement, in which case the raised level is of hepatic, not bony, origin. A normal plasma alkaline phosphatase activity, in cases with bone lesions, suggests myelomatosis rather than bony metastases. Hypercalcaemia may occur and also renal failure. The latter may occur as a result of Bence Jones proteinuria as well as the hypercalcaemia. Amyloidosis is also associated.
Cryoglobulinaemia Cryoglobulins are proteins that precipitate when cooled below body temperature. They may be associated with diseases known to produce paraproteins. About half of them can be shown to consist of a monoclonal immunoglobulin (usually IgM or IgG). The patient usually presents with other symptoms of the underlying disease and the cryoglobulin is found during investigation. Occasionally, intravascular precipitation may occur at temperatures above 22 C and, if the concentration of protein is high, presenting symptoms and signs may be skin lesions such as purpura and Raynaud s phenomenon. In some cases the proteinis polyclonal
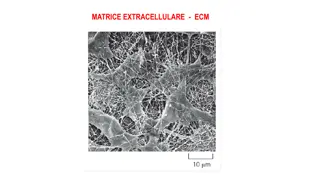
Amyloid Amyloid diseases are secondary protein structure diseases in which insoluble protein fibrils accumulate extracellularly. At least 20 different types of fibrils have been described in human amyloidosis, each with a different clinical picture. All types of tissue amyloid consist of a major fibrillar protein that defines their type are: 1-soluble in water and in buffers of low ionic strength, 2- amorphous eosinophilic appearance on light microscopy after haematoxylin and eosin staining, 3-green fluorescence seen under polarized light after Congo red staining, 4- regular fibrillar structure as observed by electron microscopy, 5- X-ray diffraction shows b-pleated sheet structure.
PROTEINS IN URINE The loss of most plasma proteins through the glomeruli is restricted by the size of the pores in, and by a negative charge on, the basement membrane that repel negatively charged protein molecules. Alteration of either of these factors by glomerular disease may allow albumin and larger proteins to enter the filtrate. Low-molecular-weight proteins are filtered even under normal conditions; most are absorbed and metabolized by tubular cells. Normal subjects excrete up to 0.08 g of protein a day in the urine, amounts undetectable by usual screening tests. Proteinuria of more than 0.15 g a day almost always indicates disease.
Renal proteinuria 1-Glomerular proteinuria is due to increased glomerular permeability, as in nephrotic syndrome. Albumin is usually the predominant protein in the urine. 2-Transient proteinuria Transient proteinuria may be associated with physical exertion, trauma, cardiac failure, fever and other acute illness. 3- Orthostatic ( postural ) proteinuria Proteinuria is usually more severe in the upright than in the prone position. The term orthostatic or postural has been applied to proteinuria, often severe, which disappears at night. Overnight urine collection shows normal albumin excretion (i.e. less than 50 mg during the 8-h period). It appears to be glomerular in origin and is most common in adolescents and young adults, typically those who are tall and thin. It may be associated with severe lordosis. Renal function is normal and proteinuria is usually less than 1g/day
4-Microalbuminuria Sensitive immunological assays have shown the normal daily excretion of albumin to be less than 0.05 g. Patients with diabetes mellitus who excrete more than this, but whose total urinary protein excretion is normal , are said to have microalbuminuria and to be at greater risk of developing progressive renal disease than those whose albumin excretion is normal. This can be assessed from the urinary albumin to creatinine ratio (ACR) The incidence of this complication may be reduced by optimization of glycaemic control and also blood pressure using angiotensin-converting enzyme. Microalbuminuria can also occur in other diseases, such as inflammatory bowel disease or rheumatoid arthritis. 5-Tubular proteinuria Tubular proteinuria may be due to renal tubular damage from any cause, especially pyelonephritis. If glomerular permeability is normal, proteinuria is usually less than 1 g/day and consists mainly of low-molecular-weight globulins and not albumin.
alpha-globulins and -globulins are sensitive markers of renal tubular damage. Tubular proteinuria can be diagnosed by measuring certain low-molecular-weight proteins in urine, such as retinol-binding protein (RBP), N-acetyl-b-D-glucosaminidase or a lpha1-microglobulin. However, because the 2-microglobulins in urine are unstable, other proteins, such as RBP, may be better indicators of tubular damage 6-Overflow proteinuria This occurs when proteins of low molecular weight are filtered normally by the glomerulus and reabsorbed at the proximal tubule but are produced in amounts greater than the reabsorptive capacity of the proximal tubule. Overflow proteinuria can be due to the production of BJP, to severe haemolysis with haemoglobinuria, or to severe muscle damage
7-Nephrotic syndrome An established case of the nephrotic syndrome is characterized by proteinuria, hypoalbuminaemia, oedema and hyperlipidaemia. The clinical condition is caused by increased glomerular permeability, resulting in a daily urinary protein loss of, by definition, more than 3 g