LATE INTRAUTERINE FETAL DEATH AND LATE INTRAUTERINE FETAL DEATH AND
Late intrauterine fetal death and stillbirth are significant concerns in obstetrics, requiring careful diagnosis and management. Real-time ultrasonography is crucial for accurate assessment, with potential secondary features indicating underlying causes. Discussions with the woman and her support network, along with thorough clinical investigations, are essential for tailored care. Recommendations for women with late intrauterine fetal death include considerations for Rhesus D-negative status and potential fetal-maternal hemorrhage. Understanding these complexities is vital for optimal outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
LATE INTRAUTERINE FETAL DEATH AND LATE INTRAUTERINE FETAL DEATH AND STILLBIRTH STILLBIRTH Prof . Maysoon sharief
Background Background stillbirth :a baby delivered with no signs of life known to have died after 24 completed weeks of pregnancy . IUFD refers to babies with no signs of life in utero. in the UK stillbirth rate was 3.9 per 1000. >1/3 of stillbirths are SGA ,1/2 unexplained 1/2 with suboptimal care.
Diagnosis Diagnosis History Examination Real-time ultrasonography is essential for the accurate diagnosis of IUFD. A second opinion should be obtained whenever practically possible. Offer repeat scan If the mother reports passive fetal movement after the scan to diagnose IUFD. If Imaging technically difficult, (maternal obesity, abdominal scars and oligohydramnios), views can be augmented with colour Doppler of the fetal heart and umbilical cord.
Diagnosis Diagnosis other secondary features for IUFD might be seen: spalding sign, hydrops and gross skin oedema unrecognisable fetal mass due to maceration. Intrafetal gas (within the heart, blood vessels and joints) occult placental abruption.
discussing the diagnosis and subsequent care discussing the diagnosis and subsequent care If the woman is unaccompanied, offer should be made to call her partner, relatives or friends. Discussions should support maternal/parental choice. offer written information to supplement discussions.
The general principles of investigation The general principles of investigation Clinical assessment and investigation : assess maternal wellbeing including: coagulopathy. risk of DIC: 10% within 4 weeks of late IUFD, rising to 30% thereafter. Tests should be repeated twice weekly in women who choose expectant management. pre-eclampsia, chorioamnionitis placental abruption. determine the cause of death, the chance of recurrence.
recommendations for women with an IUFD who are rhesus D- negative Kleihauer test for RhD-negative women to assess FMH. Anti-RhD should be administered and dose should be adjusted according to Kleihauer test. The baby s blood group can be obtained from the baby or cord or using (ffDNA) from maternal blood.
Eitology Eitology Antepartum conditions include : congenital malformation, congenital fetal infection, antepartum haemorrhage, pre-eclampsia maternal disease such as diabetes mellitus.
Eitology Eitology Intrapartum conditions include: placental abruption. maternal and fetal infection. cord prolapse. idiopathic hypoxia acidosis uterine rupture.
Transplacental infections associated with IUFD include: Cytomegalovirus. Syphilis. Parvovirus. Listeria. Rubella. Toxoplasmosis. herpes simplex. coxsackievirus, Malaria parasitaemia Ascending infection, with or without membrane rupture, with Escherichia coli, Klebsiella, Group B Streptococcus, Enterococcus, mycoplasma/ureaplasma, Haemophilus influenzae and Chlamydia are more common infectious causes in developed countries.
The best practice guidance for cytogenetic analysis of the baby The best practice guidance for cytogenetic analysis of the baby Written consent should be taken. Samples from multiple tissues are used to increase the chance of culture. More than one cytogenetic technique should be available. Culture fluid should be stored in a refrigerator and thawed thoroughly before use. 6% of stillborn babies will have a chromosomal abnormality. Some abnormalities are potentially recurrent.
the guidance on perinatal postmortem examination the guidance on perinatal postmortem examination Postmortem examination provides more information than other tests. Individual, cultural and religious beliefs must be respected when offering postmortem examination. Written consent must be obtained. Parents should be offered a description of the procedure and the appearance of the baby afterwards.. Discussions should be supplemented by the offer of a leaflet.
Postmortem examination should include : Birth weight, External Autopsy Microscopy X-ray Placenta and cord. Parents who decline full postmortem might be offered a limited examination such as needle biopsies, but these are much less informative. Ultrasound and (MRI) should not be offered as a substitute for conventional postmortem. MRI can be a useful adjunct to conventional postmortem.
timing and mode of birth timing and mode of birth Options for timing and mode of birth depends on: the mother spreferences her medical condition previous intrapartum history. immediate delivery is concidered if there is sepsis, preeclampsia, placental abruption membrane rupture Well women with intact membranes and no evidence of DIC or bleeding should have the option of immediate delivery versus expectant management because > 85% of women will labour spontaneously within three weeks of diagnosis Women who delay labour for > 48 hours should be advised to have testing for DIC twice weekly. Women with expectant management should be advised that: the value of postmortem may be reduced. The baby's appearance may deteriorate. Vaginal birth is the recommended mode of delivery, but CS may be considered with some. Vaginal birth can be achieved within 24 hours of induction of labour in about 90% of women.
IOL for a woman with an unscarred uterus IOL for a woman with an unscarred uterus Combination of mifepristone and a prostaglandin preparation are recommended as 1st line for IOL Mifepristone reduce the time interval by about 7 hours compared with regimens not including mifepristone. misoprostol use for late IUFD should be adjusted according to gestational age: 100 micrograms 6-hourly before 26 weeks; 25 50 micrograms 4-hourly after 26 weeks or more. Misoprostol and prostaglandin E2 have equivalent safety and efficacy with lower cost for misoprostol. vaginal misoprostol is as effective as oral but associated with less adverse effects(GIT, shivering and pyrexia)
IOL for a woman with an scarred uterus IOL for a woman with an scarred uterus should be undertaken by a consultant obstetrician. Mifepristone alone increase the chance of labour significantly within 72 hours: 200 mg three times a day for 2 days. Or mifepristone 600 mg once daily for 2 days. In women with a single LSCS, IOL with prostaglandin is safe but not without risk. Women with two LSCS the risk of IOL is only a little higher than for women with a single previous LSCS. Women with more than two LSCS deliveries or atypical scars the safety of induction of labour is unknown.
What are considered suitable facilities for What are considered suitable facilities for labour labour? ? Women with uncomplicated IUFD should be monitored in a separate labour room with a companion, away from the sounds of other women and babies. Care in labour should given by an experienced midwife. What are the recommendations for intrapartum antimicrobial therapy? Women with sepsis should be treated with intravenous broad-spectrum antibiotic. Routine antibiotic prophylaxis should not be used. Intrapartum antibiotic prophylaxis for women colonised with group B streptococcus is not indicated. Are there any special recommendations for pain relief in labour? Diamorphine should be used in preference to pethidine. Epidural anaesthesia should be available after assessment for DIC and sepsis.
Puerperium Puerperium thromboprophylaxis Women should be routinely assessed for thromboprophylaxis, but IUFD is not a risk factor. Heparin thromboprophylaxis should be discussed with a haematologist if the woman has DIC. suppression of lactation Cabergoline is superior to bromocriptine. Dopamine agonists should not be given to women with hypertension or pre-eclampsia. Who should be informed of events? All staff responsible for care of the woman during pregnancy and afterwards should be informed of events. All existing appointments should be cancelled.
What is best practice for use of interventions that might aid psychological recovery? Carers should be aware of to possible variations in individual approaches to death. Counselling should be offered to all women and their partners and other family members. Parents should be advised about support groups.
What advice should be given about fertility? What advice should be given about fertility? Information about fertility and contraception should be offered to mothers before returning home. Mothers are vulnerable to psychological disorders when conception occurs soon after the loss. Some women not be aware they might conceive before their first menstrual period.
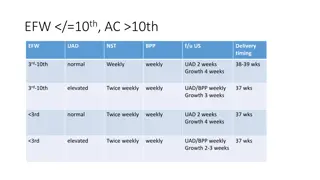
What are the recommendations for the content of the follow-up appointment? the cause of late IUFD, chance of recurrence and any means of preventing further loss. General prepregnancy advice: support for smoking cessation and to consider weight loss if BMI>25. benefit of delaying conception until severe psychological issues have been resolved. The meeting should be documented for the parents in a letter that includes an agreed outline plan for future pregnancy. Recommendations for pregnancy following unexplained stillbirth Carers should ensure they read all the notes of stillbirth thoroughly before seeing the woman. Women with a previous unexplained IUFD should be recommended to: have obstetric antenatal care. have screening for gestational diabetes. serial assessment of growth by ultrasound biometry if the stillborn was SGA.
Recommendations for the management of future delivery after unexplained stillbirth birth at a specialist maternity unit. Maternal request for scheduled birth should take into account: The gestational age of the previous IUFD, previous intrapartum history the safety of induction of labour. Recommendations for maternal care after the next birth aware for postpartum depression particularly if women conceived within <12 months from IUFD maternal bonding can be adversely affected.